Panic has spread with the discovery of a bacterium, Escherichia coli, in the United States that is resistant to the last bastions of antibiotics.
This “superbug”, which causes many common infections such as urinary tract infections, cannot be treated with the antibiotic colistin. This is the treatment usually reserved for life-threatening bacterial infections that are resistant to other antibiotics in our arsenal.
Why is this case so concerning?
Bacteria have shown many cunning ways of resisting the killing power of even our newest antibiotics. International health authorities and health-care providers have been tackling this growth in resistance for some time now. In 2014 the World Health Organisation labelled it “a major risk to public health”.
Since the discovery of “superbugs” in humans in 1968, the rise of the multi-resistant (resistant to most available antibiotics at the time) golden staph resulted in public outcry and the enhancement of efforts to use antibiotics more wisely. This is also the case for multi-resistant tuberculosis. This disease requires very toxic antibiotics and, despite some success with new antibiotics, has a high death rate.
In the case of staph, there were concerted international efforts to find new antibiotics, which temporarily allowed these serious infections to be treated. Despite these advances, staph remains a major risk for hospital-acquired infections, especially in the setting of surgery or patients with immune suppression.
Since then, we have unfortunately seen antibiotic resistance spread to many other bacteria. In fact, for every antibiotic discovered since the early days of penicillin, the bacteria have found ways to overcome their effects. Many bacteria today have multiple resistance mechanisms.
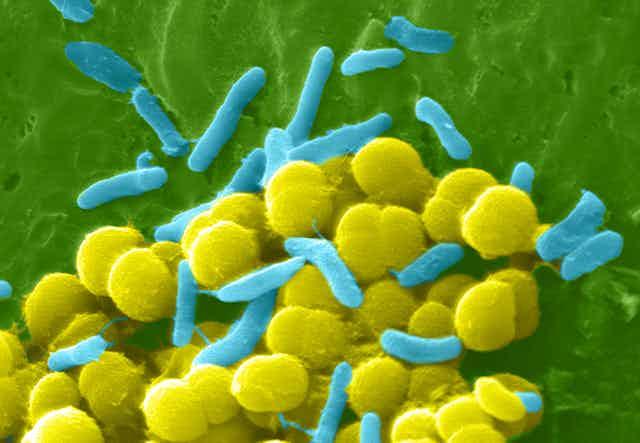
Escherichia coli belongs to a group of bacteria called “gram-negative organisms”. This group is responsible for many of the serious infections found in our most critically ill patients in intensive care. Gram-negative bacteria are particularly prone to developing and sharing resistance genes via “plasmids”, which bacteria use to share information.
Why isn’t ‘stewardship’ of antibiotics happening?
Anti-microbial stewardship is the main solution that has been put forward for the last two decades. This involves the prudent use of antibiotics to ensure they are used only in cases where they are necessary and in the most efficient way so as to avoid overuse. While this sounds good in principle, it is more complex to implement in practice as there are many barriers to successful antibiotic stewardship.
The restricted use of certain antibiotics needs to spread to all sectors including farming, where the development of resistance in animals can spread to humans. It also needs to be a global effort, as global traffic today makes it very plausible that resistant bacteria can travel too, often in patients who may not even be aware they are ill.
The public and medical community need to partner in the avoidance of antibiotics unless there is indication they are necessary. Often the fear of serious infections leads to the over-use of antibiotics. Adherence to the treatment program is also important. This concerted effort is what makes stewardship so difficult.
How do we tackle this problem before it’s too late?
The World Health Organisation estimates 50% of all antibiotics consumed globally are used to treat or prevent infections in animals. These antibiotics make their way into the public as residues in the food consumed or during preparation in contaminated food products.
In 1969, the Swann Report raised the concern of the widespread use of antibiotics in farming. In 2003, the Institute of Medicine issued a warning that sub-therapeutic doses of antibiotics in animal feed can cause resistant bacteria to develop.
The problem is widespread. Chicken, pork and farmed fish receive antibiotics such as tetracyclines that are also used to treat infections in humans, and antibiotics like avoparcin that cause cross-resistance to similar antibiotics used in humans.
In October 1999, the Joint Expert Technical Advisory Committee on Antibiotic Resistance report outlined the size of the problem in Australia. After multiple committees, working groups, implementation groups and multiple summits, there has been only partial movement on some of the recommendations and no progress on several key recommendations.
In 2000, Denmark banned antibiotic use in agriculture. There are lessons to be learnt from the Danes’ success.
More recently, there’s been policy noise from lobby groups looking to enhance public health efforts and funding to develop new options to treat and prevent multi-resistant infections.
Researchers around the world are looking at innovative ways to tackle the problem. New antibiotics are unlikely to solve the problem unless new antibiotic classes are developed. This is unlikely if one looks at current medications in development by pharmaceutical companies. Only a handful of drugs will be reaching the market in the next decade, and most will be similar to existing antibiotics.
There are economic barriers to antibiotic development, with pharmaceutical companies opting instead for the lucrative markets of oncology and chronic diseases.
New approaches include enhancing the killing capacity of the immune system for certain bugs. Lessons from cancer research have shown us the immune system can sometimes be “paralysed” by certain bacteria, such as Legionella. If the system can be tweaked with targeted drugs, then the body’s own immune system will help fight the infection.
Another option is to optimise the choice of antibiotic through more accurate and reliable testing in patients with suspected infections. This will allow doctors to choose their antibiotics more wisely. If doctors are able to use tests that pinpoint the bug causing a patient’s infection, they will be able to use the right antibiotic and thus reduce the chances of resistance.
Innovative research will require appropriate government support. So far we have been relatively spared multi-resistant organisms, but for how long? This remains everyone’s problem to solve.