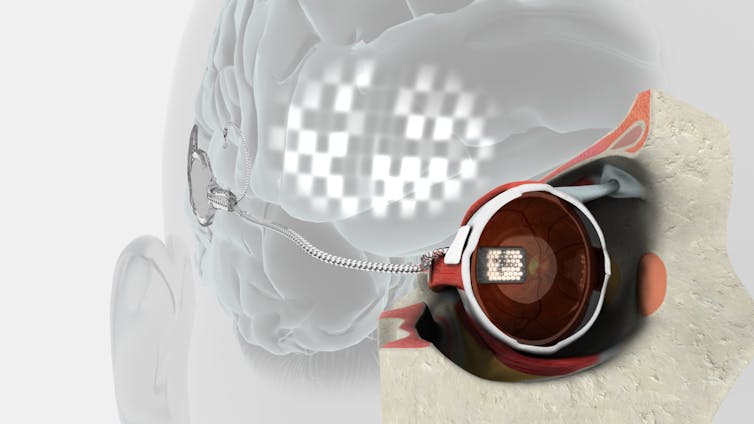
Visual prostheses, or “bionic eyes”, promise to provide artificial vision to visually impaired people who could previously see. The devices consist of micro-electrodes surgically placed in or near one eye, along the optic nerve (which transmits impulses from the eye to the brain), or in the brain.
The micro-electrodes stimulate the parts of the visual system still functional in someone who has lost their sight. They do so by using tiny electrical pulses similar to those used in a bionic ear or cochlear implant.
Electrical stimulation of the surviving neurons leads the person to perceive small spots of light called phosphenes. A phosphene is a phenomenon of experiencing seeing light without light actually entering the eye - like the colours you may see when you close your eyes.

These phosphenes in someone with a bionic eye can be used to map out the visual scene. So the vision provided by a bionic eye is not like natural sight. It is a series of flashing spots and shapes the person uses to interpret their environment through training - somewhat like a flashing mosaic.
Currently, the vision provided by a bionic eye is very basic and can be used for tasks such as identifying the location of an object, detecting a person, or finding a doorway. Researchers hope future bionic eye devices will provide higher resolution vision, but this has inherent challenges.
How the bionic eye works
A bionic eye converts images from a video camera (left picture below) to a high-contrast representation (middle picture), of which a portion is selected for further processing. This is the blue-shaded box below, corresponding to the reduced field-of-view of a typical bionic eye.
An external video processor then converts this high-contrast image to electrical stimulation parameters, which are sent to electrodes implanted in the eye. The bionic eye recipient perceives a blurred image (right of the picture) comprised of flashes of light.

What recipients actually see
We know from the experience of our Melbourne patients that activity on the electrodes is seen as a series of bright flashes rather than as a steady perception. The world is thus flashing bursts of light arranged to represent the basic shape – like the height and width – and approximate location of an object in front of the camera. Other recipients have said this was like:
looking at the night sky where you have millions of twinkly lights that almost look like chaos.
Recipients need to use these irregular flashes to interpret the camera image. The field of view (the extent of the observable world) is small – about 30 degrees wide or one hand span at arm’s length – so recipients need to have a good memory to put the whole image together.
Improvements to the external camera and video processing are able to assist here. For example, distance-sensing cameras can highlight obstacles such as a rubbish bin on the sidewalk, and thermal cameras can highlight human shapes. Right now, the best outcomes rely heavily on patient engagement and rehabilitation.
Who gets a bionic eye?
The type of bionic eye that may be an option for patients is dependent on the cause of their vision loss. Retinal bionic eye implants are placed into the eyeball itself, and are only suitable for people who have lost their vision from specific diseases such as inherited types of retinal degeneration known as retinitis pigmentosa and age-related macular degeneration.
Read more: Explainer: what is age-related macular degeneration?
To date, only people with degenerative retinal diseases have been eligible to receive a bionic eye. Three retinal bionic eyes have been approved for commercial sale: the Argus II developed in the USA, the Alpha-AMS in Germany, and the IRIS V2 in France.
We ran clinical trial with three people, between 2012 and 2014, using a new device developed in Melbourne, Australia. This device may have a safer surgical profile than existing bionic eyes as it is implanted at the back of the eye rather than inside the eye.
Prior to surgery, the Melbourne patients would not have been able to see a hand waving in front of their face. With the bionic eye implant, they were able to locate objects on a table, and navigate around objects in their path while walking, demonstrating that the implant could provide useful visual information in the real world. We are preparing for a trial of a second-generation implant in the next year. These are all retinal implants and have mainly been used for people with retinitis pigmentosa.
Implants placed on either the optic nerve or directly into the brain may be able to provide benefit to people with a broader range of conditions, such as trauma or glaucoma. Devices for these particular conditions are still in the research phase but are expected to enter human clinical trials in the near future.
Read more: Explainer: what is glaucoma, the 'sneak thief' of sight?
The quality of vision with a retinal implant heavily depends on the residual eye health of the patient and the ability to interpret the created phosphenes. The implanted electrodes aim to replicate the function of missing light sensitive cells (photoreceptors). But there must be viable surviving neurons for the electrodes to interact with.
Another complicating factor is that there are many neuron types in the retina but the electrodes are too large to selectively target individual types. For this reason, bionic eyes cannot replicate the sense of colour. In fact, artificial vision is very different from normal vision and takes a lot of getting used to.
Can image quality be improved?
At present, there are several approaches to improve image quality. One is to increase the number of implanted micro-electrodes and make them smaller, allowing them to target selective neurons for more independent “pixels” and greater resolution. There are newer nanotechnology materials that might allow the electrodes to be small enough to produce high-acuity resolution.
Another technique is to refine the electrical stimulation patterns to better focus the stimulation to activate smaller-sized clusters of neurons. We can also artificially increase the resolution by creating “virtual electrodes” where electrical current is shared between two or more electrodes. These new stimulation methods could improve stability, reduce blurriness and possibly even provide rudimentary control over colour.
Ultimately, researchers are seeking to understand and mimic the neural code the retina uses to communicate with the brain. If the firing patterns of photoreceptors could be replicated, the correct message would be transmitted to the brain. The resulting vision would become significantly more natural.
Read more: Some people can't see, but still think they can: here's how the brain controls our vision
Combining these techniques, the level of vision attainable might allow patients to independently navigate around without the use of a guide dog or cane. It could be possible to recognise everyday objects or even emotions on faces of loved ones. As to which approach is ultimately feasible, only time will tell. One thing that is certain is bionic eyes will get better over time.

