If you thought that vaccine hesitancy was the biggest challenge of the pandemic, think again. A new challenge is approaching: supply chain hesitancy. The potential for interruption along vaccine supply lines may lead to pauses in vaccination rollouts that will affect millions of people.
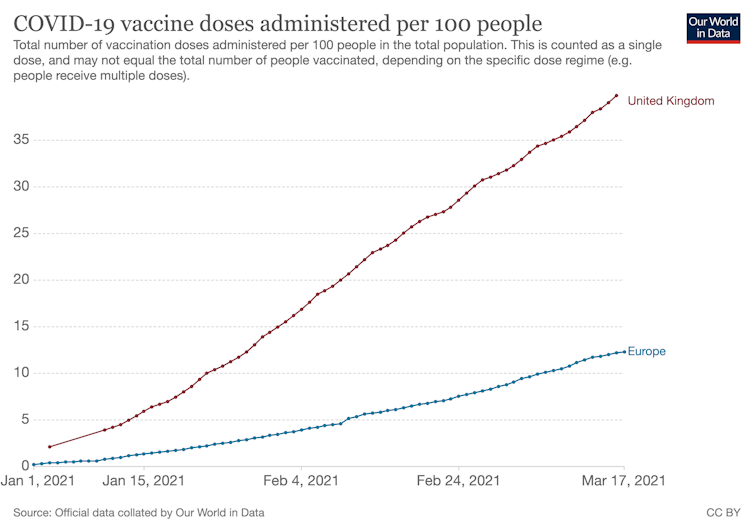
In the UK, the government’s Joint Committee on Vaccination and Immunisation has warned of a delay in under-50s getting immunised, partly because of supply issues with the AstraZeneca vaccine. Meanwhile, the EU, where many countries temporarily suspended the AstraZeneca rollout due to reports of blood clots, has threatened to restrict exports of the vaccine if supply in Europe does not improve. We await a clear European response.
So far, more than 25 million people in the UK have received their first dose of a COVID-19 vaccine. But the ongoing supply for the remainder of the month into April is now seriously at risk with the delivery of first and certainly second doses now subject to uncertainty.
While cross-border discussions and disputes unfold around the AstraZeneca vaccine in particular, it is likely that this problem is also being heavily affected by both political and public health concerns.
Successive lockdowns have made people more aware of how products and services move along a supply chain. Home deliveries of food, furniture, clothes, and any number of other things can be very easily tracked, monitored and confirmed from the supplier to our front doors. Digital supply chains are the norm, and information about demand, supply, orders and returns is now almost instantaneous.
So how is it that we might be facing a sudden halt to the vaccine rollout in the next few weeks in the UK?
Immunisation at scale is a highly complex challenge – and the global supply chains that will aid this are also intricate. No modern supply chain can totally avoid disruption. But in an age where there are many techniques to overcome a stop-start in supply chains (called “lumpy demand”), what might the effects of this be on the current challenges that the AstraZeneca supply chain is facing and what options do vaccine suppliers and governments have?
Supply and demand
In operations management, we normally teach our students about two types of supply chain problem. First is the “bullwhip effect”, which concerns rapidly dwindling supply in response to demand shocks. Suppliers struggle to keep up with demand further down the chain and end up running out of product, commonly referred to as “stock-out”.
Then there is the “Osborne effect” – named after the early 1980s laptop manufacturer that went bust rapidly after raising consumer expectations of a newer product that rendered its current device obsolete overnight. This example is also not a good outcome, as the supply chain grinds to a halt with large amounts of unused stock held in warehouses.
What the UK government has outlined is ultimately a bullwhip effect of lumpy demand and supply – a brief pause between production and distribution of vaccine batches which will have a knock-on effect on expectations about supply.
Nonetheless, in both cases, the solution is one of understanding both supply and demand – adjusting the dynamics of supply and the actions of all the relevant people involved along the way, in order to match demand needs. In this way, it’s possible to level out the lumpy demand, balance the expectations of supply and generally coordinate a smooth flow of products.
If this transpires to be a minor blip, or if another hurdle is encountered in terms of distribution to the UK and EU, then we may be faced with a different but equally important challenge: take-up and rollout of vaccination being impinged by trans-border regulation, political arguments and the decisions of medical regulators. Yet even in this case, this would have nothing at all to do with supply chains.
How to fix the problem
The current issues the UK and EU are facing are related to India’s Serum Institute and the availability of manufacturing ingredients. These issues of materials supply are immediately solvable, though impacted still by availability and multiple regulatory requirements.
The overall solution is either to increase supply or to stabilise demand through increased prioritisation and reducing the speed of vaccination – or a variation of both. Contractual commitments should not be affected, citizens should be assured, inter-governmental arguments should not rear their head.
This, of course, is not what’s happening. The global economic impacts of the pandemic, the physical and mental health effects of COVID-19, poverty and social inequalities all threaten to destabilise the vaccine rollout, especially now elements of the political economy are becoming increasingly involved (as in the case of Brexit).
But this should not deter us.
The UK is still at the forefront of a successful vaccination rollout at speed, and at scale – that should be highly commended.
The most important things now are to focus on sticking to the plan, ensuring vaccine delivery occurs rapidly when the frequency of supply can be assured again and – most importantly – shifting to a more agile supply chain mindset. That means governments and pharmaceutical companies need to work together in order to meet demand and supply as it changes, putting measures in place to assure a steady supply of vaccine in order to alleviate any concerns.
To ensure future supply chain problems do not occur, we strongly recommend both pharmaceutical companies and national governments think ahead to ensure COVID-19 vaccine supply chains are given priority support in terms of their ability to respond to shocks and “chokes” in supply and demand – devoid of political interference.
We cannot afford to take our foot off the gas now. Our citizens and our supply chains will not thank us for it. We will be answerable to future generations about what we could have done to turn the tide against the pandemic. That’s not a question we want to get wrong.

