Britain’s badgers stand on the brink of being shot, gassed or even forcibly fed oral contraceptives, all in the name of fighting the spread of tuberculosis in cattle. But what dangers does bovine TB (as it is known) really pose? Does this disease or others like it pose a threat to human public health?
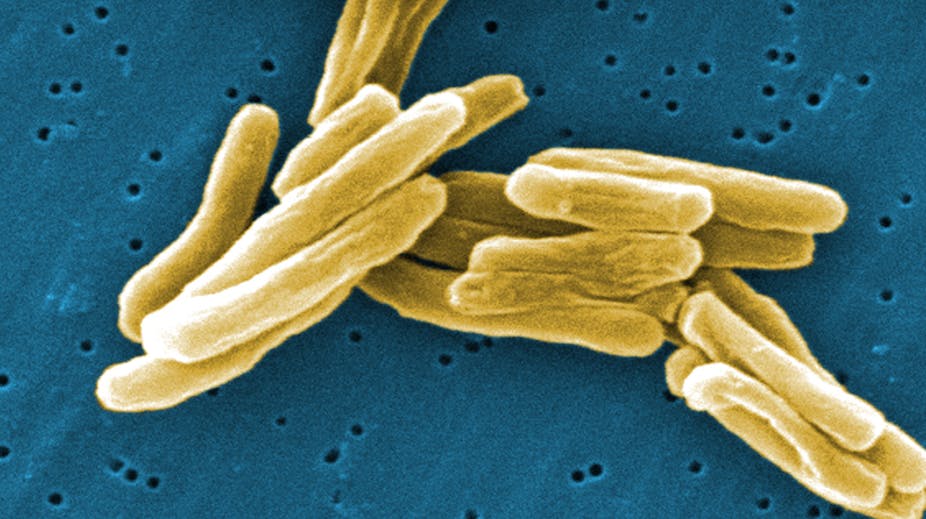
Tuberculosis (TB) is one of the oldest diseases of humans and mammals. Modern-day TB originated from a hardy environmental pathogen that could survive in the hot dusty climate of East Africa. When humans moved out of Africa 15,000 years ago, TB went with them and adapted as a specialised human pathogen known as Mycobacterium tuberculosis. Around the same time, with the development of agriculture and animal husbandry, TB also specialised into a strain adapted to live in cattle, Mycobacterium bovis. A disease that can move between different species in this way is known as a zoonosis.
The two TB strains are closely related, and although they have a preferred host, bovine TB has been found in many mammals, including humans - and badgers. In Europe, where milk was a main food source for thousands of years, many people believed in the connection between contaminated milk and human disease. By the turn of the 20th century, TB was the cause of between one in four and one in six deaths in Europe, and infection was endemic among the urban poor of the now industrialised world. As around a third of cattle in Britain were infected, establishing whether there was a link to infection in humans was of paramount importance.
In 1901, the British Congress on Tuberculosis debated the relationship between bovine TB and human infection. The world-renowned bacteriologist Robert Koch presented experiments which showed that cattle did not become infected when injected with human TB. This, he argued, demonstrated that bovine TB and human TB were distinct diseases and that it was not necessary to take any measures against bovine TB in humans.
But Koch was wrong. It was finally established that humans were susceptible to M. bovis, and between 1912 and 1937 65,000 cases of TB in humans were attributed to bovine TB. Pasteurisation of milk removed it as a route for human infection, with only three recorded cases of TB in humans from milk in 30 years. The test-and-slaughter eradication scheme in cattle which began in the 1950s had by 1980 cut cattle-to-cattle infection rates to record low levels.
Figures show that direct transmission of bovine TB to humans is rare but not impossible. Of the 30 human cases of bovine TB per year, around half come from consuming unpasteurised dairy products and around 40% from direct exposure to cattle. Human-to-human transmission is rare - one example came in 2005 with a cluster of six cases contracted in a Birmingham nightclub and traced back to a young farmer out on the town. In general, the rise in cattle cases has not been accompanied by a rise in human cases and it is certainly not the threat it once was.
While bovine TB is a well-known zoonotic infection, other zoonotic pathogens are only just being identified. One particular bacterium that is not often thought of as a zoonotic pathogen is Staphylococcus aureus, better known as Methicillin-resistant Staphylococcus aureus (MRSA) due to its resistance to the penicillin family of antibiotics. MRSA is a global health problem, particularly in causing hospital-acquired infections. However, S. aureus has long been known to cause infections in livestock, such as mastitis in the udders of dairy cattle.
In 2005 a new type of MRSA associated with livestock called ST398 was identified. Initially identified in French pig farmers, it has now been widely reported in pigs and other livestock, and in farmers, vets and slaughterhouse workers in contact with livestock. It’s also been found in cow’s milk in the UK (don’t worry: the pasteurisation will kill it). Small outbreaks of ST398 have taken place in the wider human population, such as at a nursing home and a hospital ward in the Netherlands. The success of ST398 as a pathogen has actually increased the overall burden of MRSA infections in some countries in Europe.
Of particular importance is that many ST398 strains found in livestock and people in close contact with livestock are resistant to tetracycline antibotics, widely used in livestock production. Strains of the bacteria isolated from people with no contact with livestock are not resistant to tetracycline. This suggests the resistance to the drug stems from its farming use.
In the UK, the vast majority of zoonotic pathogens reach us via food. Some zoonoses are rare but serious and cause huge public concern, like variant Creutzfeldt–Jakob Disease (vCJD) which has been linked to the consumption of cattle infected with Bovine Spongiform Encephalopathy (BSE). Other zoonoses cause milder but more widespread infections, like Campylobacter jejuni, which is transmitted to humans via eating undercooked poultry and is the most common cause of food poisoning in the UK, causing over 70,000 cases a year.
One thing is clear from our current understanding of zoonotic infections past and present, is that human and animal health are inherently linked. Often the focus of research is human pathogens, but we need to maintain a watchful eye on both human and animal infectious diseases in order to be able to anticipate and manage new threats as they emerge.