Australian researchers have shown for the first time that the number of girls presenting with pre-cancer cells on the cervix has dropped following the introduction of a wide ranging vaccination program.
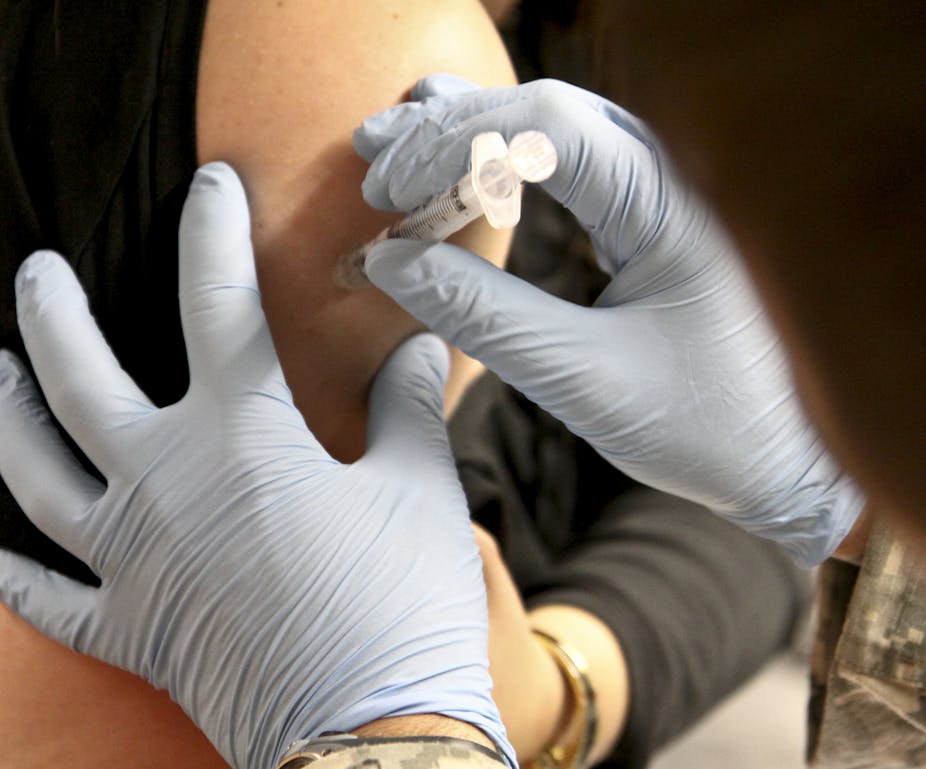
Under an Australian scheme launched in 2007, all girls and women aged 12 to 26 were encouraged to be vaccinated against the human papillomavirus (HPV), the sexually-transmitted virus that is the primary cause of cervical cancer.
Critics of the scheme have argued that vaccinating girls against the virus could encourage promiscuity.
However, a new study showing that the program was followed by a drop in the number of girls presenting with high-grade cervical abnormalities (a cancer precursor requiring biopsy), will boost arguments in favour of large scale vaccination schemes.
“There’s no doubt in a country like Australia, where we have been extremely fortunate in having a highly successful screening program, one of the main benefits of vaccination to those girls and women who have been vaccinated is the chance to reduce the risk of having an abnormal pap test result,” said lead researcher, Dr Julia Brotherton from the Victorian Cytology Service Registries.
“That then reduces the need to go on and have biopsies and further treatment. I certainly would rather have a needle than have an abnormal pap test result and a biopsy so it’s very encouraging news.”
Using data from the Victorian Pap Test register, the researchers compared the incidence of cervical abnormalities before and after the vaccination program began.
A trend soon emerged. Following the introduction of the vaccination, the incidence of high grade abnormalities in girls aged 17 years and younger fell by 0.38% compared with before the vaccination program (from 0.80% to 0.42% among screened women, a decline of nearly 50%).
“The fact that we are seeing the change in the younger women certainly supports the theory that it is the vaccine causing this effect,” said Dr Brotherton.
The study has been published in the medical journal The Lancet.
Dr Brotherton stressed that further research was needed.
“Although we can say it’s a statistically significant decline, we can’t necessarily say it’s due to the vaccine. It could be due to other factors such as changes in the types of women presenting for screening or changes in diagnosis,” she said.
Professor Michael Quinn, an expert in gynaecologic oncology at the University of Melbourne, also said more work needed to be done.
“The study is the first anywhere to show falling rates of high grade change in very young women and although this is likely to be due to the effects of the vaccination program, further analysis of information linking women’s smear history to their vaccination history will be needed to prove that the fall is entirely due to vaccination rather than other factors,” he said.
However, Associate Professor Karen Canfell, an epidemiologist with the Cancer Council NSW who advised the researchers on methodology, said the study underlined how important it is that parents of 12-13 year old girls have their daughters vaccinated.
“The study is also a timely reminder that even if women have been vaccinated, they will still need to have regular cervical screening, because the vaccine does not protect against all types of HPV that are implicated in cervical cancer,” she said.
“Cervical screening, combined with vaccination, is still the best way to prevent cervical cancer.”