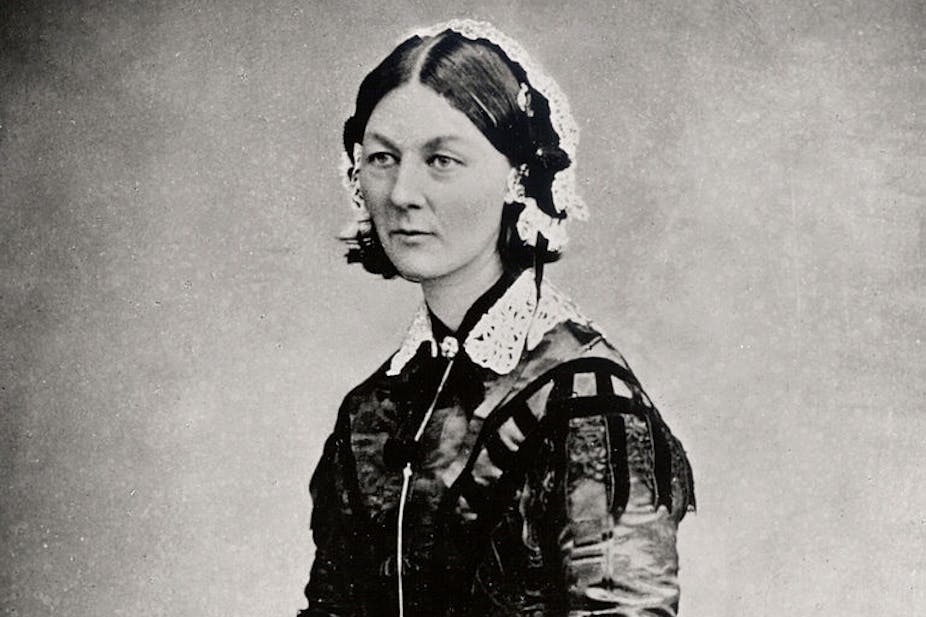
What would Florence Nightingale make of present-day healthcare? Like anyone else, she would probably find much to admire – even much to be in awe of – but just as much of which to disapprove and despair.
We might reasonably assume she’d appreciate our technology and be greatly heartened by the extraordinary leaps made on this front that allow more time to be spent with patients. One of the cornerstones of her philosophy, after all, was that healthcare is about “nursing the sick, not nursing the sickness”.
But she would be mistaken. It’s more accurate to say technology serves principally as a means of treating more patients, and is mainly used to get the conveyor belt they travel on to go faster. As the first female member of the Royal Statistical Society, Nightingale would surely discern as much if she were to set about familiarising herself with the metrics, targets and production-line methodologies that have come to dominate our way of working. It is also very likely that she would also detect the alarming reduction of the one characteristic she cherished above all others: compassion.
Nightingale might well pity her modern-day successors, the members of the profession she did so much to shape, who are habitually blamed for a lack of compassion when things go wrong.
Selective memory
“Compassion” was one of the healthcare buzzwords of 2013. The problems at Mid-Staffordshire, where shocking failings led to unnecessary deaths and appalling levels of care, made it so. But by and large, interpretation of what compassion is and why it is relevant has been decidedly selective; while the importance of compassionate qualities in individual nurses has been much discussed, compassionate qualities in the healthcare system as a whole has gone strangely unremarked.
In truth, compassion should be central to the very broadest strategies. It should be fundamental not only to people but to process and place. In other words, it should be a focus not just for those who work within the NHS but for those who manage its services. Existing business-style models of management tend not to lend themselves to such seemingly lofty ideals. Optimisation and efficiency are frequently at odds with the basic notion of finding time to think, talk, identify with and understand.
Restoring humanity
But there is hope. The pernicious influence of threat and blame, assembly line mentalities and the pursuit of benchmarks, workflows and trajectories as an end in itself is at last earning a measure of wider recognition – the Francis Inquiry report, which examined the causes of the failings at Mid-Staffordshire was one high-profile example. But recognition is also taking place more privately, as people, professionals and organisations grow increasingly disillusioned, amply indicated in a recent blog at the King’s Fund.
Far less appreciated, however, is how we sort out this problem. Education is one obvious answer. New public management thinking in recent decades – the language of business and bureaucracy – condemned the language of care to the margins. We’re now crying out for a renewed, and much greater, emphasis on how nurses can contribute in creative and practical ways to the design of compassionate interventions, processes and spaces. Something that reaches right back to Nightingale’s philosophy.
Physical surroundings also have a part to play. The workplace itself has to be conducive to compassion. Emotionally “warm” clinics are innately better than “cold” ones. Hospitals might usefully rediscover the concept of hospitality – not just for those they treat but for those who deliver the treatment. The pioneering Maggie’s Centres are a great example of this.
Whatever the specific answers might be, the overall goal should be to restore humanity to healthcare. The transformation doesn’t have to be inherently radical or, worse still, prohibitively expensive. It’s not so much a question of money: it’s a question of mindset.
More than a minute spare
Ultimately, what we need is a major move away from the current credo, which is that compassion is some sort of ointment that smiling practitioners can apply in the few seconds they have to spare. Healthcare is unworthy of the “blip culture” that Alvin Toffler presaged more than a quarter of century ago, where encounters are limited to short “blips” often of five minutes or less across multiples sites.
Compassion has to be systematic. And the message (and a framework) needs to come from the top. Everyone needs to be on board, it’s not just something that can be relied on to ascribe culpability to a single group.
Nightingale was revered as a role-model, an inspiration, the embodiment of all that’s noble and human about nursing; by contrast, the nurses of today are treated as little more than scapegoats. That’s how things have really changed: she carried a lamp and they carry the can. And that can’t be right.