Genetic traits like a bulbous nose or balding give some people reasons to moan about what they inherited from their parents. But more serious genetic flaws can cause debilitating disease. Now, Italian researchers have come up with a way of treating one such inherited disease and reversing another using a promising new method of gene therapy.
The idea behind gene therapy is to replace a faulty gene with a shiny new version that works properly. Modified versions of viruses, which have been sculpted by millions of years of evolution, perfectly penetrate human cells. They act as couriers delivering DNA payloads to defective cells and ensure it is stably inherited.
This deceptively simple idea, though, has been challenging to achieve in practice. The first commercial gene therapy product, Glybera, only received regulatory approval in 2012.
Part of the reason for this is the difficulty of successfully clearing three hurdles at once: delivering replacement genetic information to the exact cells that need help, getting this information safely translated in high enough volumes to overcome the defects and stopping the immune system from reacting to “normal” genes when it has grown used to only seeing mangled ones.
Now, a team led by Alessandra Biffi at the San Raffaele Scientific Institute in Milan, Italy reports in the journal Science that they have developed a new approach that navigates each of these hurdles to treat three children with metachromatic leukodystrophy (MLD), a devastating inherited disease that affects around 1 in 40,000 people.
Engineered stem cells
MLD usually manifests in early childhood and kills patients just a few years after the first symptoms appear. It is caused by a defect in a single gene, ARSA. This gene encodes information used by the lysosome, a piece of recycling machinery used by human cells to break down unwanted material. When this recycling process does not work properly in nerve cells, as is the case with MLD patients, they become filled with rubbish and begin to slowly decline, leading to brain and spinal cord degeneration, as well as sensory deprivation.
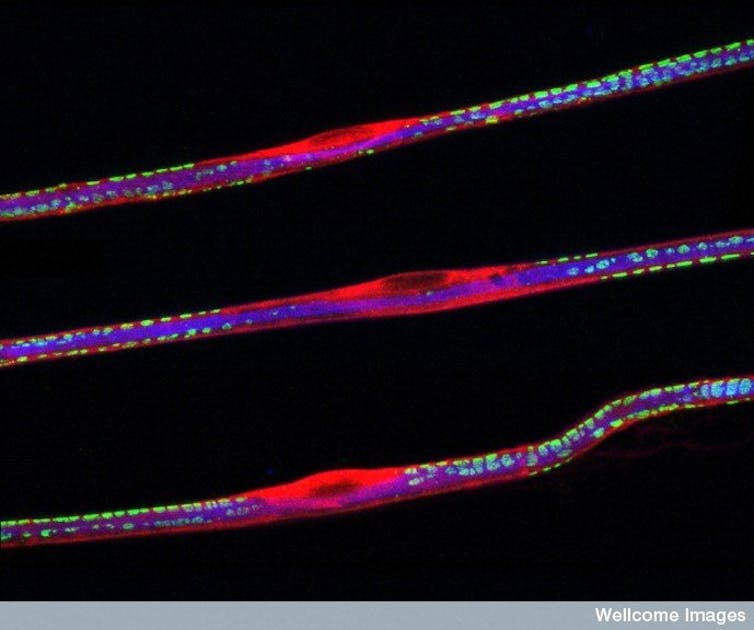
Supplying a replacement ARSA gene to affected cells in the nervous system is a tricky task, because these areas are heavily protected. To overcome these defences, the team employed haematopoietic stem cells (HSCs), which can usually be found nestling quietly in the bone marrow, as stealthy genetic couriers. A tiny number of these cells were harvested from each patient, loaded with benign viruses carrying a working copy of ARSA and put back into the bloodstream.
These engineered cells either lodged in the bone marrow or continued to travel around the body in the blood, where they corrected defective cells in the nervous system by supplying the normal version of ARSA. Because these were stem cells, they also reproduced to form new blood cells that themselves took on the same supportive roles.
Resurrecting lysosomes from the dead
Most MLD patients produce a garbled version of ARSA that has a very low level of activity, nowhere near enough to let the lysosome carry out its normal job. Restoring partial activity is not enough to make a clinical impact – levels must be hiked to make an obvious difference.
One way of maximising activity is to pack defective cells with lots of normal copies of the same genetic message. In this case, haematopoietic stem cell couriers were loaded with two to four copies of the same virus, introducing multiple reproductions of the normal ARSA gene into the host cell genome.
To check that these viral inserts did not cause any unintended biological disruptions, which could lead to very serious side effects (like leukaemia), every individual founder cell infused into the patients was tracked using a genetic barcode. While some original cells generated large pools of daughter cells early on, which could be a sign of dangerously uncontrolled growth, none of them continued to dominate the blood cell pool as time went by.
In the patients, levels of ARSA quickly skyrocketed to above-average concentrations in both the original courier stem cells and their progeny. More than a year after treatment, normal ARSA levels were detected in the cerebrospinal fluid of all three patients, a clear sign that the central nervous system had stabilised. All these kids, who have older siblings badly affected by the same disease, can now think, run, jump, sit, crawl, kneel, jump, roll and speak like similarly aged average preschoolers.
Using the same technique, in a separate paper in Science, a team led by Alessandro Aiuti of the same institute in Italy showed reversal of the Wiskott-Aldrich syndrome (WAS) in three other young patients.
Like MLD, WAS is also a disease caused by a defect in a single gene. The disease causes immune system dysfunction that leaves kids at high risk of infections, bleeding and being harmed by their own immune system. But HSCs loaded with viruses containing the correct version of the faulty gene were able to restore a properly functioning immune system.
Using this stem cell-based gene therapy technique, both these new studies have either prevented the onset of a serious neurodegenerative disease, or reversed existing immunological disease. These are a testament to the tremendous potential of gene therapy and they represent a great step towards long-lasting cures for single-gene diseases.

