Following a public vote, the 2014 Longitude Prize to develop an idea that will help solve one of the greatest issues of our time will go to a project working on antibiotic resistance. The focus of the £10m award will go to the best idea for a cheap, fast and accurate detector for bacteria and their associated antibiotic resistance mechanisms that could help better guide treatment.
Antimicrobial resistance is one of the most serious health threats to the global community. Microbes that are resistant to multiple classes of antibiotics are the cause of common infections including skin and soft tissue infections, urinary tract infections, pneumonia, diarrhoea and sexually transmitted infections.
Added to this, multi-drug resistant bacteria are making it increasingly difficult to treat infections in vulnerable or at risk groups like the elderly, organ transplant patients and premature babies. Globally, resistance in microbes that cause tuberculosis and malaria, Candida (a fungus that commonly causes serious infections in hospitalised patients) and viruses such as HIV and influenza is prevalent and on the rise. It’s not a pretty picture.
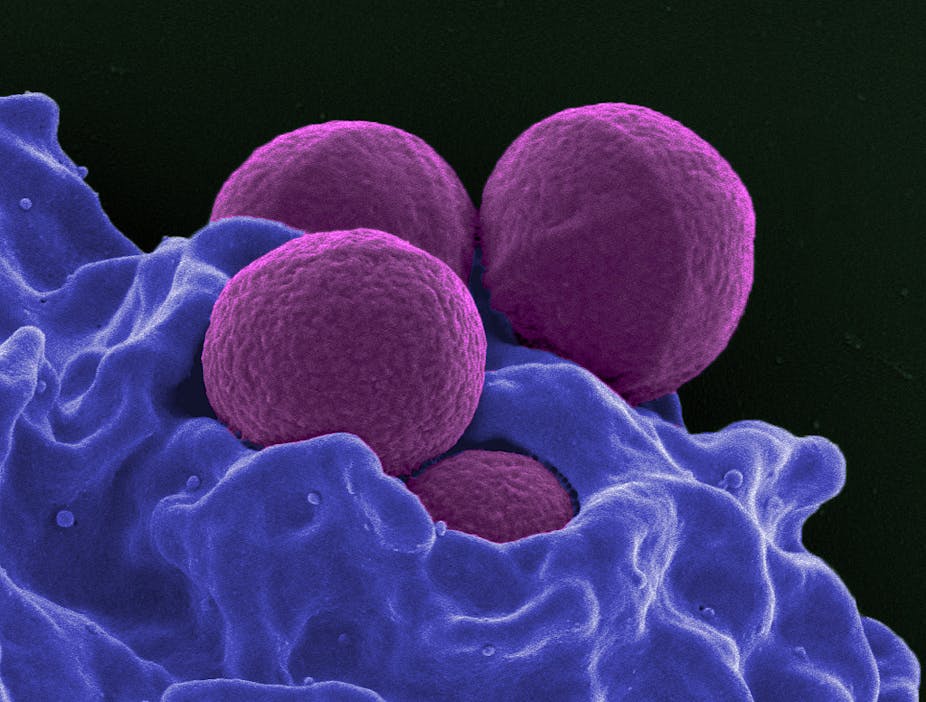
In the US, the Centers for Disease Control (CDC) conservatively estimates that more than 2m illness are caused by antibiotic resistant bacteria and fungus each year with 23,000 associated deaths – mostly in hospitals and other medical settings, although they can occur anywhere. Methicillin resistant Staphylococcus aureus, more commonly known as MRSA, was associated with more than than 80,000 invasive infections in 2011. Clostridium difficile, a bacteria that causes severe recurrent diarrhoea, is linked to antimicrobial use and resistance and estimated to be associated with 250,000 illnesses and 14,000 deaths every year.
Antibiotic-resistant organisms develop from selective pressure caused by the use of antibiotics during patient therapy or in food animals. The CDC has proposed four core actions to fight the spread of antibiotic resistance, including tracking resistant bacteria, improving the use of antibiotics, and promoting the development of new antibiotics and new diagnostic tests for resistant bacteria.
All of these actions are crucial to controlling global spread and discovering new ways to treat antibiotic resistant microbes. Health care providers need to prescribe appropriately and patients need to finish their full course of therapy so that bacteria don’t have the opportunity to survive and develop resistance.
But diagnostic testing to rapidly identify microbes and their resistance genes is one feasible option that could improve targeting of antibiotic drugs. This approach would pave the way for more intelligent antibiotic use. Currently, initial therapy of an infection is often empirical, with antibiotics selected to treat the most common microbes associated with that type of infection.
Rapid diagnostics could also help the effort to detect and prevent the spread of antibiotic resistant organisms. Diagnostics are being developed by groups and companies in a bid to reliably detect numerous pathogens from a single biological sample and the presence or absence of genes that encode for antibiotic resistance.
While diagnostics will be an important part of helping us to move beyond resistance, the discovery and development of new antibiotics and therapeutics that target the ability of microbes to cause infections are critical. This is based on a more basic understanding of how these organisms cause infections via the secretion of toxins that disrupt the human immune system or direct toxicity to host cells, which is the case with MRSA and C. difficile infections. This is important to the development of new therapeutics that can target these molecules and increase the efficacy of currently available antimicrobials.