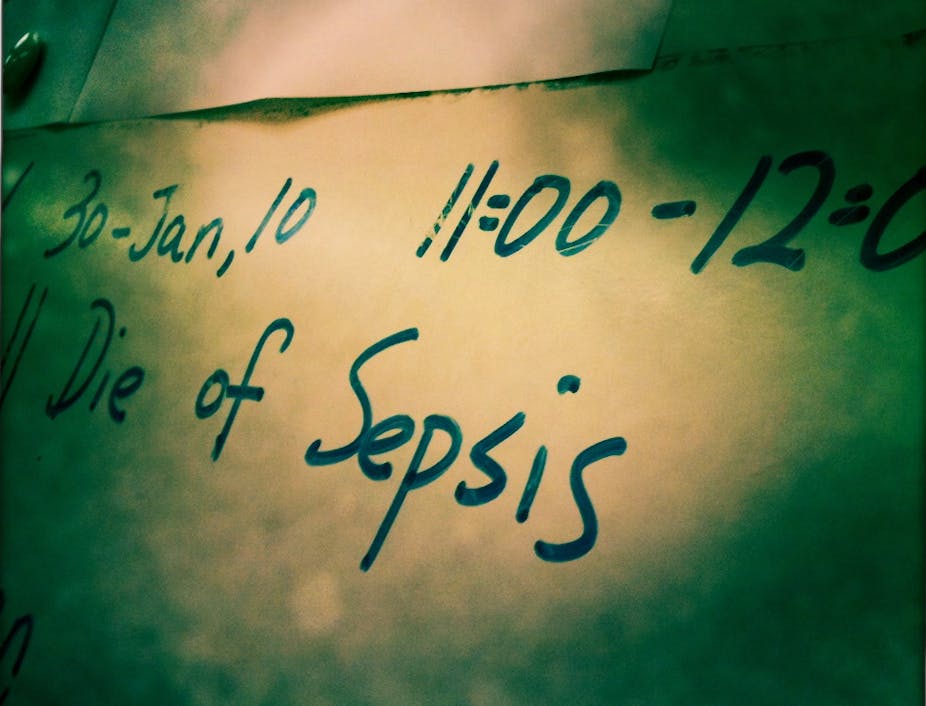
Sepsis claims the lives of 8m people worldwide each year. It is the leading cause of hospital deaths in the US, a major threat to soldiers wounded in battle and a killer of children, particularly in under-resourced areas around the world.
Sepsis occurs when bacteria, fungi or viruses multiply in a patient’s blood and trigger a chain reaction that causes inflammation, blood clotting, and organ damage. Traditional treatment requires doctors to race against the clock to pinpoint the specific type of pathogen causing the infection so that the right antibiotic therapy can be administered. But in many cases blood cultures never make a positive identification, so we often treat them blindly.
Patients generally receive broad-spectrum antibiotics along the way, but things often go downhill fast and can end in septic shock, where blood pressure drops to dangerous levels. This is a challenge made greater still by the growing population of antibiotic-resistant superbugs and viruses where we currently have no treatment at all.
But there is some hope. Here at Harvard’s Wyss Institute, we are hot on the trail of the sepsis problem. In collaboration with other Harvard colleagues and two hospitals, we’ve developed a dialysis-like therapeutic device that could radically transform the way doctors treat sepsis, which we announced in Nature Medicine.
Meet ‘the biospleen’
The “biospleen” is a device inspired by the human spleen, which filters pathogens and toxins from flowing blood without requiring doctors to identify the pathogen causing the problem – and it captures antibiotic-resistant bacteria as well. We found that it was able to remove more than 90% of bacteria from the blood of rats in a few hours. It also increased survival when these animals were injected with a lethal bacterial toxin.

The biospleen works outside the body like a dialysis machine. It consists of two hollow channels that are connected to each other by a series of slits: one channel contains flowing blood and the other has a saline solution. Key to its success are tiny nanometer-sized magnetic beads that are coated with a genetically engineered version of a natural immune system protein called mannose binding lectin (MBL).
The magnetic beads are added to the blood after it flows from a patient’s vein and before it enters the device. After the beads bind to pathogens, they are pulled from the flowing blood, through the slits, and into the neighbouring saline channel by a magnet in the device, which cleans the blood before being returned to the patient.

Best of all? The device simply and effectively cleans the blood without the need to first pinpoint the pathogen responsible for the infection because the MBL protein binds to more than 90 different causes of infection and sepsis, including bacteria, fungi, viruses, parasites and toxins.
Getting ideas out of the lab
Very innovative and potentially groundbreaking ideas often get stuck in the mire of traditional academic laboratories because they cannot be validated to the degree required by financial investors, for example, by working through manufacturing and regulatory challenges.
At the Wyss Institute, we’ve teamed up in-house inventors, engineers and entrepreneurs to speed up the commercialisation of our technologies. They’ll work with the blood cleansing device to get it out of the laboratory as soon as possible to begin saving lives.
The major reason no-one ever explored this idea in the past is that most clinicians and researchers assume that because blood cultures are negative, there are no circulating pathogens. But the reality is that there is circulating dead pathogen debris and many toxins, which are primary triggers of the inflammatory cascade that leads to sepsis. The power of this device is that it binds to dead pathogens and toxins as well as live bugs.
The next step will be to test and validate the technology in large animal studies and from there into human clinical trials.