Researchers have created a pain-free DNA vaccine skin patch that tests on monkeys show is over 100 times more effective than a normal needle at kicking off the first step in getting a DNA vaccine to work.
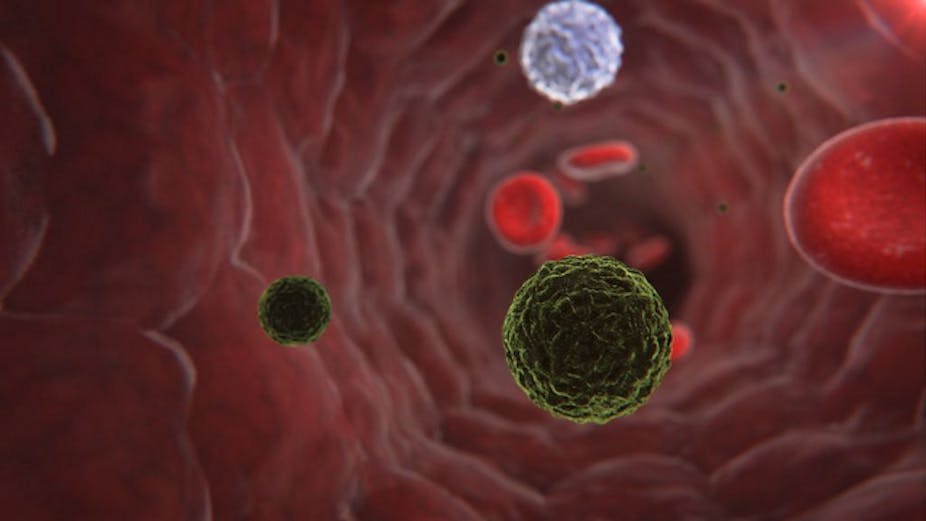
DNA vaccines are a relatively new form of immunisation and work by injecting a small amount of a germ’s modified DNA into a person.
The germ’s DNA is then taken up by cells in the person’s body and expressed for a short time to produce an antigen, which kicks off the production of antibodies and killer T cells that fight disease.
Scientists hope that DNA vaccines could one day protect us from HIV, malaria and dengue fever but the technique’s success has been limited so far because human cells are not usually very effective at taking up the germ’s DNA and starting the disease-fighting process.
A new study, published in the journal Nature Materials, found that in tests on monkeys called macaques, swapping normal needles for a specially designed DNA vaccine patch with microneedles so small they are barely visible to the eye could markedly improve the vaccine’s effectiveness.
“DNA vaccines have many potential benefits but have failed to generate robust immune responses in humans,” wrote the researchers, who are based at MIT and Harvard in the United States.
To combat the problem, the researchers developed a patch that, over days and weeks, uses tiny needles to deliver the vaccine through several layers of skin – similar to the way a tattooist’s needle penetrates several layers of skin.
“But the important distinction is that there is no pain with the microneedle approach as opposed to tattooing,” said lead author of the paper, Peter C. DeMuth from the Department of Biological Engineering at the Massachusetts Institute of Technology in the US.
“It’s also important that in our work we’ve designed an approach that allows for the microneedles to only be applied for 15 minutes to deposit vaccine depots into the skin. These vaccine depots can then present vaccine to the patient’s immune system over longer time periods.”
In other words, the painless microneedles quickly dissolve, leaving behind a film that releases the vaccine over the following days and weeks.
The researchers said that “when applied to viable macaque skin ex vivo, multilayer tattooing elicited 140-fold greater gene expression compared to naked DNA injection.”
“Thus, this polymer film tattooing approach may offer a route to efficacious DNA vaccines via a pain-free and self-administrable dry skin-patch platform,” their paper said.
Professor Robert Booy,a vaccine expert and Head of Clinical Research at the University of Sydney’s National Centre for Immunisation Research and Surveillance said the finding was very interesting.
“This paper brings together two remarkable technologies – DNA vaccines and microneedle patches –into one new approach, where the whole is greater than the sum of the parts,” said Professor Booy, who was not involved in the research.
“It’s an approach where, potentially, people could no longer need a doctor or nurse to inject a vaccine but could apply it themselves without any pain, needle-phobia or risk of cross infection.”
Unlike normal vaccines, the DNA vaccine patches would not need refrigeration, which would drive down costs and allow them to be administered cheaply, said Professor Booy.
“Essentially, the scientists have found a way to hit the immune sweet spot and thereby hit the bugs for six, over the boundary and out of the body.”
Many common vaccines work by modifying a live germ so it is harmless but still capable of stimulating the body’s immune response. However, the risk remains that a live vaccine could mutate into a dangerous strain.
“With DNA vaccines, that can’t happen,” said Professor Booy, who added it was important to remember the new patch had not yet been tested on humans.
“As with any fantastic concept, there are a huge number of steps from imagination to effective delivery. Consider penicillin, which was discovered in 1928 but not shown to be effective until 1942,” he said.