The National Institute for Health and Care Excellence (NICE) has published new draft proposals laying out major changes to the way it assesses whether new medicines offer value for money for the NHS. These evaluations are difficult – requiring as they do an assessment of the value of life – but are necessary in all healthcare systems that face spiralling costs worldwide. The new proposals, however, could prevent or delay new and effective drugs from reaching patients with cancer.
The draft proposals show that NICE, the body that decides which drugs are available on the NHS in England and Wales, plans to change the parameters its appraisal committees use
End-of-life criteria
Under the current system, NICE gives extra weight in its evaluation of cost-effectiveness if drugs have shown a particular benefit in patients at the end of their lives. The calculations it uses are complex but essentially, if a drug has been shown to add three months of life expectancy to patients who have an incurable illness then the NHS may pay a price significantly higher than it would otherwise pay to roll it out.
The importance of end-of-life criteria is very clear: since 2009, when they were introduced, 12 cancer drugs have been approved on this basis. It is likely that many of these drugs would have been rejected in the absence of end-of-life criteria. The new system proposes to remove the criteria, instead incorporating end-of-life benefit into a broader, less defined measure of what would qualify for a higher price bracket. This risks fewer drug approvals in future.
In addition to removing end-of-life criteria from the drug appraisal system, NICE has also suggested it will remove specific consideration of how innovative a new treatment is. I worry that both of these changes will result in cancer drugs being rejected when under the current system they would have been approved. This could deny cancer patients access to life-extending drugs and dramatically reduce the likelihood of achieving the cancer cures of the future.
At The Institute of Cancer Research in London, we have direct experience of the value of the current drug approval process. For example, a groundbreaking new prostate cancer drug called abiraterone that we discovered has helped thousands of sufferers. Initially approved for patients with late-stage prostate cancer resistant to existing drugs, abiraterone has since gone on to benefit patients in earlier stages of the disease. Yet abiraterone would probably not be approved under the proposed changes.
Stifling innovation risk
By omitting specific consideration of innovation, the new guidelines will discourage the more creative, high-risk drug discovery research. Previously, NICE’s cost-benefit analysis allowed innovation to be rewarded by paying more for innovative drugs, although the definition of innovation was quite loose. In the new proposals, the chance to formalise the importance of developing novel treatment types has been overlooked. The consequences could be very damaging.
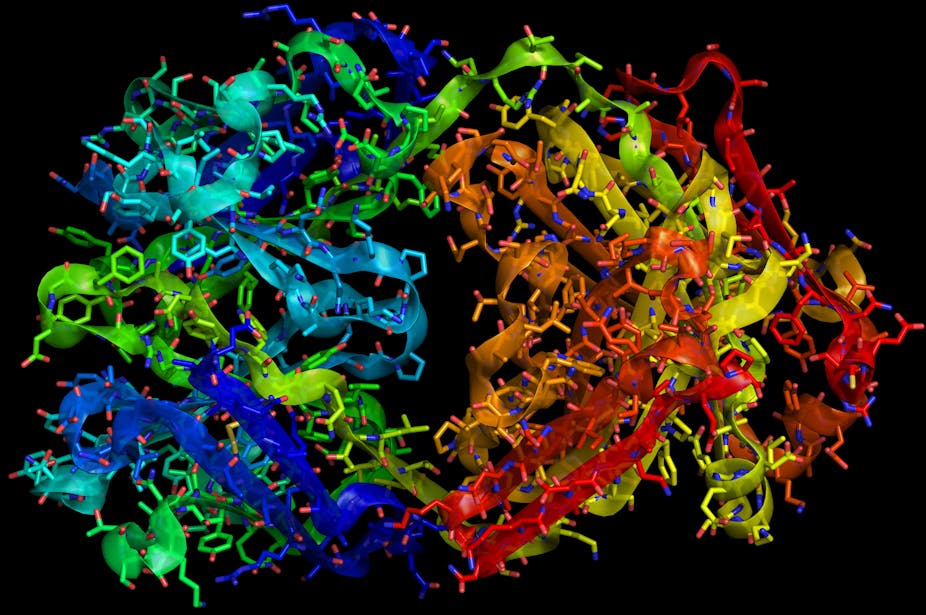
Innovative cancer drugs are those with new mechanisms of action – particularly precision medicines that act on new molecular targets derived from basic cancer biology research and the latest genomics studies, and also those that exploit cutting edge immunological research. Innovative drugs are tremendously important because they offer the possibility of major breakthroughs that cannot be achieved with those that simply mimic or marginally enhance the effects of existing drugs.
In recent years, our understanding of cancer has increased dramatically and we’ve learnt that cancer medicine works best when it is personalised to individuals. One of the best examples of developing this kind of personalised, precision medicine is trastuzumab. This has helped extend the lives of breast cancer patients with high tumour levels of the HER2 marker, a protein which drives the growth of their cancer. HER2 is also important in a proportion of stomach cancers and NICE approved trastuzumab use in these patients on the NHS under the old end-of-life criteria. Again, this might not have happened under the new draft proposals.
Tackling drug resistance
Innovation is also essential if we are to overcome the massive problem of drug resistance – the most important challenge facing cancer drug discovery and development today. We now know that resistance arises because cancers are extraordinarily variable and versatile in evolving mechanisms to get around the effects of both molecular targeted and conventional drugs.
An example of an innovative approach to tackle resistance is the discovery and development of Hsp90 inhibitors – a totally new type of drug that we, and only a few other research centres worldwide, have pioneered. These inhibitors have the exciting ability to target several different cancer molecular weaknesses at once, and so can overcome or even prevent drug resistance.
It took costly, high-risk research to develop Hsp90 inhibitors and they have progressed from being a poorly appreciated drug target to one of the most actively pursued in the drug industry today. Leading Hsp90 inhibitors have shown very encouraging results in trials of patients with HER2-positive breast cancers that have become resistant to trastuzumab and patients with non-small cell lung cancer who have become resistant to the widely used molecular targeted drugs erlotinib and crizotinib.
It would be very disappointing if this sort of innovation is not rewarded when it comes to deciding if the NHS will pay so that patients can benefit.
Another crucial benefit arising from both the end-of-life criteria and the current guidance that promotes innovation is that drugs originally approved for “end-of-life” use very often turn out, later on, to benefit patients with earlier stage cancer – as noted above with abiraterone. Also, the current system provides an initial route into the NHS for innovative drugs, which can then subsequently be shown to be effective in the harder-to-treat cancers, especially by combining them with other drugs. New drug combinations could hold the key to tackling drug resistance for many cancers and encouraging innovation is critical for this.
Crucial time
The proposed NICE changes could mean a backward step at a crucial point in the history of cancer drug discovery and development, research and development costs of which are of course very high. Clinical trials are the most expensive part and failure in these is still depressingly common. But the high costs and failure rates are mostly a result of the old one-size-fits-all approach where potential drugs are not targeted to the specific molecular characteristics of individual patients.
The costs of developing personalised drugs will eventually fall because clinical trials supporting drug approval will be smarter, smaller and shorter. Instead of relying on a small number of one-size-fits-all blockbusters, companies will have a larger portfolio of lower volume, personalised precision drugs that are targeted to smaller patient populations. The transition to personalised drugs with reduced prices will take time, but this must happen.
Nonetheless, it’s a hugely exciting time, both in basic cancer research and in creative drug discovery and development. We must not let overly restrictive regulation deprive patients of access to innovative and life-prolonging drugs that are being developed now and in the future.