Getting a new pharmaceutical from an idea in the chemistry lab to market takes many years and billions of dollars. Each year just several dozen new drugs are approved for use in the United States.
Human “organs-on-chips” are leading a revolution in drug safety testing. These devices use human cells to model the structure and function of human organs and tissues. By testing the potential effects of drugs on different organs faster than traditional methods, organs-on-chips can reduce the need for animal studies and better predict which new drugs will effectively treat human disease.
As part of an interdisciplinary research team with funding support from the National Center for Advancing Translational Sciences, we’re working on a kidney-on-a-chip to improve our understanding of how kidney diseases begin and which drugs can safely treat them.
Quicker and better testing
Historically, laboratory testing for new drugs is performed in cells grown in dishes or flasks. If a drug passes initial screening tests in vitro, researchers next test it in vivo in live animals to determine the effects of a new drug on a whole system instead of just one cell type at a time. Finally, after many years of laboratory investigation, researchers will test a promising new drug in people to see if it is safe and effective.
The problem is 9 out of 10 of these drugs never make it from small-scale human tests to the patient because they turn out to be ineffective or toxic, even if they showed promising results in early testing.
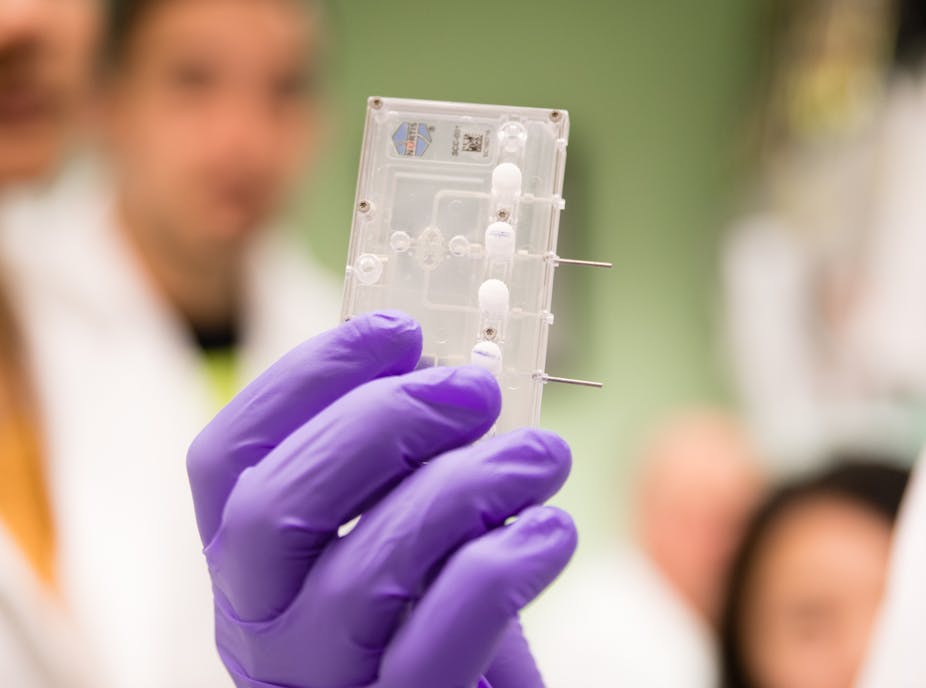
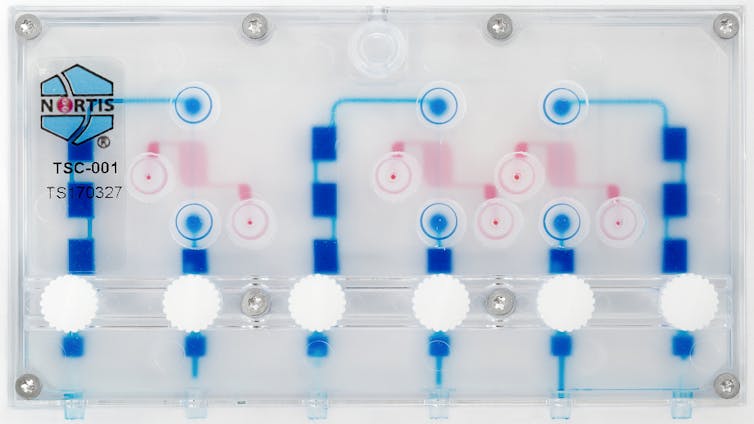
Organs-on-chips have the potential to completely transform that system. Ranging from the size of a fingernail to that of a credit card, they’re composed of fluid channels and tiny chambers that contain human cell samples. Organs-on-chips in development in labs around the country include kidney, lung, liver, intestine, skin, brain, heart, bone and reproductive systems.
In an organ-on-a-chip, flowing liquid supplies the cells with oxygen and nutrients, similar to the way blood sustains cells in the human body. It’s this constant flow that makes these devices special. Cells grown in organs-on-chips devices act more like cells in a human organ than do cells grown in flat dishes without flow.
Case of the kidney-on-a-chip
Kidneys are incredibly important to overall human health. The two fist-sized kidneys remove drugs and unwanted compounds from the body and play a critical role in maintaining proper salt and water balance, blood pressure and vitamin D and bone health. Genetic conditions and even commonly administered medications can, in some circumstances, damage the kidneys.
In the U.S., 15 percent of adults have kidney diseases. But most don’t even know it, because kidney diseases often display no symptoms until the condition is very advanced. There’s a pressing need to understand how kidney disease begins, and to develop new safe and effective treatments.
Here at the University of Washington, our kidney-on-a-chip research team is composed of scientists from many different disciplines, including pharmacy, pharmaceutical sciences, nephrology (kidney medicine), toxicology, biochemistry and bioengineering.
In partnership with Nortis, Inc., a local biotechnology company, our team has created a small device — the size of a business card — with up to three tiny tubes, each one-thousandth the size of a drop of water, containing 5,000 human kidney cells. When tiny amounts of fluid are pumped through the tubes, the kidney cells are exposed to important signals that help the cells in the chip behave as if they were in a live kidney.
We’ve found that the kidney cells release signals – called biomarkers – of injury when exposed to known kidney toxins. Our research showed that cells on the chip released markers of injury commonly seen in the urine of people with kidney damage. Testing with the older method, using cells on plates, did not show any damage with the same treatment. This suggests that the kidney-on-a-chip may be better than existing methods at predicting if a new drug will cause kidney damage in humans.

Connecting organs-on-chips to mimic systems
Now that we’ve had these promising results, scientific teams across the country are starting to connect different organs together to replicate a more complex, multi-organ system, to give greater insights into how drugs affect people. For example, we were able to connect a liver-on-a-chip to a kidney-on-a-chip to learn how a plant extract used in some herbal medicines, called aristolochic acid, damages kidney cells. This chip-to-chip investigation reinforces the need for interconnected organs-on-a-chip to replicate the complex mechanics in the human body.
In the coming year, our kidney-on-a-chip project will be one of several sent to the International Space Station where low gravity speeds up changes in cells, sometimes causing health problems for astronauts. The Space Station could be the perfect place to find out more about kidney diseases in weeks, rather than years or decades.
Organs-on-chips can also be used to discover new drug targets. Our team is evaluating the kidney-on-a-chip as a tool to personalize drug selection and dosing in people with kidney cancer, polycystic kidney disease and chronic kidney disease. Other organs-on-chips labs around the country are studying diseases of the immune system, brain, lungs, heart and blood vessels. By working together, dozens of research teams are developing this new technology to revolutionize drug discovery, leading to the development of better and safer medications for all.