Codeine is the most widely available opioid analgesic in Australia, but the problems with its well-intentioned overuse are not so widely known or talked about. I was therefore delighted to see it being highlighted in a mainstream news outlet tonight. It’s not news at all to those who work with headache sufferers a lot. We have known for a long time about the phenomenon of rebound headaches from taking short-acting opioids and other headache drugs. A related but not identical problem which is what the Adelaide study was looking at is that of opioid-induced hyperalgesia. A comprehensive and free review article from a good journal about it can be found here.
The setup goes something like this…you have neck pain or migraines or some other reason to suffer headaches that occur fairly frequently. You don’t think they’re bad enough to see a GP about, but they are frequent and perhaps even a bit disabling. You begin to need the odd sick day or else you just push through at work or at home doing what you need to do in increasing amounts of discomfort.
Even if you don’t particularly like taking medication, chances are you might try some paracetamol or ibuprofen from the supermarket, and find they don’t work that well. You go the next step and ask a pharmacist for ‘something a bit stronger.’ The next rung of OTC treatment is usually a compound analgesic with either paracetamol or ibuprofen combined with a bit of codeine (usually around 8mg). Codeine itself is regarded as a ‘weak’ opioid because it only weakly interacts with the mu opioid receptor, about which more below.
Here’s the dilemma. If your headaches are helped by the codeine, you are likely to use it again, and again, and again and so on until you inevitably become more tolerant of it. If not, you may then eventually go and see a GP who may recommend another, slightly stronger codeine-containing drug with a paracetamol, a higher dose of codeine (usually 30mg) and possibly some doxylamine as well. Let’s imagine you continue to have headaches 3 or 4 days a week but a dose or two of the analgesic keeps them manageable so you can soldier on. What often happens next if you continue to rely solely on the drug to manage your headaches is that you develop a dull, moderately severe headache on the days when your ‘normal’ headaches don’t come. You will probably treat those with codeine as well.
Now you have a devilish choice to make. You probably feel a bit uneasy about taking so much pain relief so you try going without on some days and find that within a day or two your headache is crippling. Clearly, you need something for it….and so the cycle goes.
A quick bit of pharmacology..
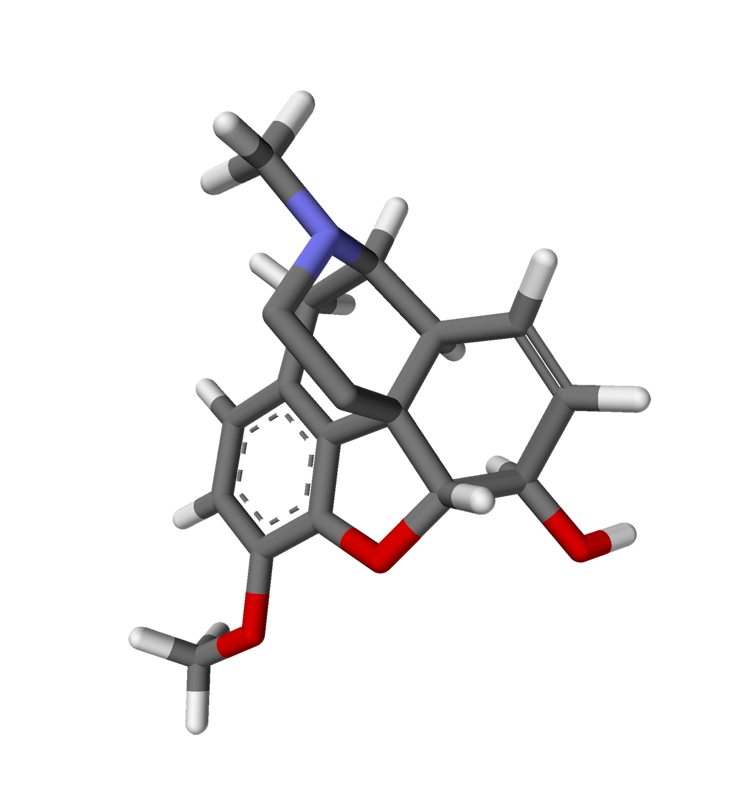
Codeine is a naturally-occurring opioid compound which can be isolated from the opium poppy juice. These days it is mostly synthesized. It derives most of its pain-relieving ability from being metabolized into morphine by the CYP2D6 enzyme system in the liver, and also from an active metabolite of its own. Genetic influences and interactions of other drugs with the CYP2D6 system mean that metabolism through this pathway is highly variable. In most people, perhaps 90% of the codeine is not metabolized into a form which can give pain relief. Hence, the pain relieving effects of codeine range from completely ineffectual (up to 25% of the population) to intoxicating (high percentage of conversion to morphine).
Despite being a ‘weak’ opioid for the purpose of pain relief, codeine interacts robustly with the other opioid receptors (the delta and kappa variety). So if you take your 30mg of codeine per tablet, you get 30mg worth of nausea, constipation, drowsiness and tolerance but only around 3mg worth of analgesia.
Back to headaches
So here’s the problem with having really freely available OTC codeine…it literally creates as many headaches as it relieves in moderate to heavy users. Treating rebound headaches involves a slow wean, or a hospital stay for infusion therapy to wean off it faster. It also demands having nonpharmacological methods of improving the headaches, such as aerobic conditioning, stress management strategies, and other CBT-type skills. It may also involve needing migraine prophylaxis or other medical investigations ina small percentage of cases.
Then you still have the original problem of the headaches, be it migraine, tension headache or any of the other few dozen types in the International Classification of Headache Disorders hierarchy. Having access to appropriate diagnosis and treatment is also a major issue in most parts of the country due to lack of neurologists and pain specialists who have the expertise to manage these common problems. But it can be well worth the effort if it saves you from suffering in increasingly desperate silence or getting stuck in a medication spiral which can’t help you in the long run.
