Seventy-five years ago, a new stimulant drug with the generic name of methylphenidate was born in the Swiss lab of chemical company Ciba. Like many drugs, its therapeutic purpose was unclear. But these were the days a scientist could take a drug home and test it on their spouse, which is exactly what Ciba scientist Leandro Panizzon did. Panizzon’s wife, Rita, reported that the drug gave her tennis game a real fillip. And so Panizzon named the drug Ritaline in his wife’s honour.
Listen to an audio version of this article on The Conversation’s In Depth Out Loud podcast:
Panizzon would not have been surprised by this. Stimulants, including amphetamines, such as Benzedrine, had been used since the 1930s for a variety of afflictions, including psychiatric disorders. During World War II, they were widely prescribed to both Allied and Axis military personnel.
In 1950, Ciba patented methylphenidate as Ritalin – dropping the “e”. But questions remained about who could benefit from it. Initially described as an “analeptic”, or health-restoring drug, Ritalin was used to treat patients recovering from drug-induced comas and anaesthesia.
Over the next three-quarters of a century, Ritalin would wear many hats, including antipsychotic, tonic for worn-out housewives, drug to treat disruptive children, street drug and smart drug.
Growing pains
Ritalin found its first home in psychiatric asylums. It was widely prescribed to chronically depressed, schizophrenic and psychotic patients, the “mentally retarded” and patients recovering from lobotomies.
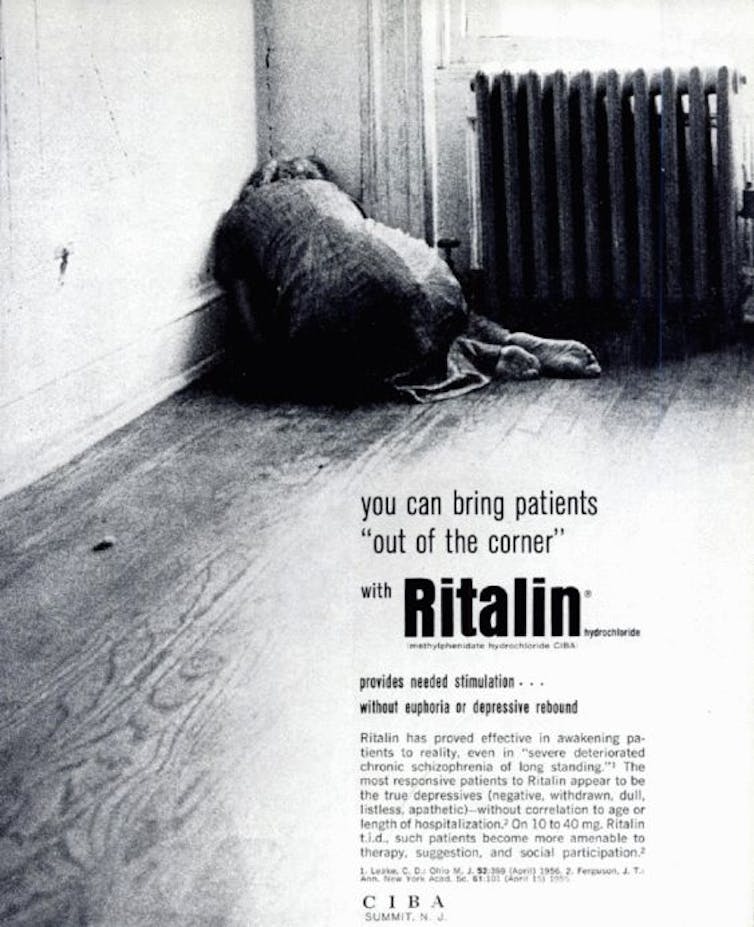
An advert from 1956 shows a woman huddling next to a radiator on a bare asylum floor, promising psychiatrists that they can “bring patients out of the corner with Ritalin”. Ritalin was thought to make patients alert enough to engage in psychoanalysis, which many psychiatrists believed to be the only route to recovery. But with asylums being shut left, right and centre, Ciba had to look elsewhere for patients.
The next patients for Ritalin were unlikely to be hospitalised. Instead, they suffered from milder symptoms, ranging from anxiety and apathy to depression and fatigue. Ads from the 1950s and 60s targeting these patients focused on the middle-aged and elderly or, as one writer put it, “oldsters” and “troublesome, miserable old people”.
One competitor Ciba faced for the “oldster” market was not another antidepressant, but a different stimulant: caffeine. A 1957 report described Ritalin as being “less potent than amphetamine, but more so than caffeine”. In advertising, Ciba also emphasised that Ritalin was a “mild” antidepressant, not as addictive as stronger amphetamines, such as Benzedrine.
A common trope in Ritalin ads during this period was the tired housewife. An ad from the 1960s depicted a before and after scenario. In the before picture, a sixty-year-old woman stares glumly at a large pile of unpeeled potatoes. In the after picture, the woman peels the last of her potatoes, though not looking particularly happy about it. The caption reads: “if chronic fatigue and mild depression make simple tasks seem this big, Ritalin relieves chronic fatigue that depresses and mild depression that fatigues”.
The potato-peel ad highlights how drugs were marketed to tackle everyday problems. With drugs like Ritalin, (but also bestselling anti-anxiety drugs and tranquilisers, such as Miltown and Valium) the message to women, in particular, was clear. Instead of dealing with the aspects of their lives that made them tired and depressed, they should turn to “mother’s little helper”.
Ciba also targeted post-partum mothers, exhausted businessmen, narcoleptics, convalescents and “oversedated” patients. One ad even promised that Ritalin could cure “environmental depression” caused by the stresses and strains of modern life. Despite these efforts, Ritalin struggled to thrive in the crowded marketplace for psychiatric drugs.
Finding its feet
In 1961, the US Food and Drug Administration (FDA) approved the use of Ritalin in a new patient type. Rather than targeting depressed, fatigued and older patients, Ciba targeted the opposite: the hyperactive child. Within a decade, Ritalin went from also-ran to bestseller.
In some families, a strange scenario would have emerged. A parent would be prescribed Ritalin to pick them up, while their child took it to calm them down. As a 1970s Ritalin ad showed, the drug had “many faces” and many patients. And while it might seem strange to use a stimulant to calm a child down, the practice had precedence.
The link between stimulants and behaviour emerged in 1937 at Emma Pendleton Bradley Home, a child psychiatric facility in Rhode Island. The medical director, Charles Bradley, had been draining the cerebral spinal fluid of patients to make better images of their brain. He gave the children Benzedrine to help treat the headaches and nausea that followed the procedure.
The drug did not ease the children’s side effects but caused “spectacular improvement in school performance” in half of them. Children became “emotionally subdued … without losing interest in their surroundings”. Bradley published his findings, recommending such drugs for treating children with behaviour problems.
For twenty-five years, few psychiatrists took notice. This was because hyperactive, impulsive and inattentive children were not of concern to either psychiatrists or teachers until the late 1950s. They were more worried about neurotic, withdrawn and inactive children – the very opposite type of child.
But attitudes changed in 1957 with the Soviet launch of Sputnik. The Soviet success in space convinced American politicians, scientists, educators and the military that the education system was broken. The National Defense Education Act was passed the following year to accelerate educational achievement.
Read more: ADHD: how race for the moon revealed America's first hyperactive children
The Act identified three ways to outpace the Soviets. First, emphasise core subjects, such as science, maths and English. Second, reduce the number of students dropping out of high school and encourage more students to go to college. Finally, hire guidance counsellors to identify children who struggle to meet these new expectations, especially those who appeared intelligent but struggled to succeed in school.
These children would become the first children diagnosed with what we would now call attention deficit hyperactivity disorder (ADHD). The term ADHD or ADD would not be coined until the publication of the third edition of the Diagnostic and Statistical Manual of Mental Disorders in 1980. But a new disorder described in 1957 would accurately describe these hyperactive, impulsive and inattentive children: hyperkinetic impulse disorder.
Before the definition of hyperkinetic impulse disorder, hyperactivity in children had to be severe to be considered problematic. Children with this disorder were rare and often suspected of having brain damage or food allergies. And they often ended up in psychiatric institutions.
The psychiatrists who defined hyperkinetic impulse disorder worked at one of these institutions – the same Bradley Home where the link between amphetamines and behaviour had been made. But the disorder they described was anything but rare. In fact, it was described as a “very common” condition found in most classrooms. Unsurprisingly, given their workplace, they also recommended the use of drugs in treating the disorder.
The first major trial into the effects of Ritalin on behaviour was conducted by Leon Eisenberg and Keith Conners, then of Johns Hopkins University in Baltimore. The results of the trial were viewed as a triumph for Ritalin. But a close analysis reveals a more complex picture. Set in a residential facility, the trial did not study schoolchildren but hospitalised children. This suggested that the behaviour being assessed was relatively severe.
The researchers also noted that, while the behaviour of the subjects improved, there were serious side effects in 70% of the children. These side effects were worrying enough to place the double-blind nature of the trial at risk. Finally, Eisenberg and Conners’ conclusion was not a blanket endorsement of the drug but a recommendation for more research. Later in life, both men expressed the view that ADHD was overdiagnosed and Ritalin was overprescribed.

Still, the newfound concern about hyperactivity combined with a newfound faith in psychiatric drugs meant that Ritalin had become a bestseller for Ciba by the late-1960s. The willingness to prescribe psychiatric drugs to children reflected a shift to biological psychiatry more generally. The influence of psychoanalysis was waning and biological psychiatrists were now occupying positions of power within American psychiatry. But psychiatrists and other physicians were also impressed with how quickly Ritalin appeared to help children.
Parents were also impressed. In a 1968 story in Time Magazine, a mother described how before Ritalin her son was impossible to control. With the help of Ritalin, she could now “love this child again”. As awareness of Ritalin grew, parents began asking their doctors for prescriptions.
Ads for Ritalin now showcased the drug’s miraculous ability to transform children. A before-and-after ad showed a blond boy tearing apart an educational toy in the “before” image. The boy is blurred, highlighting his hyperactivity. The text beside the image describes him as “being in perpetual motion”, “aggressive” and “destructive”, struggling at school despite being “bright”.
The “after” images show a profound change. The first shows the boy curled up on a sofa, transfixed by a history book. In the second, he is being embraced by his adoring mother. The message was clear: Ritalin could redeem children and repair relationships.
Midlife crisis
Despite its popularity, Ritalin quickly became controversial. Critics attacked the drug and its effects as well as what it and ADHD represented. Was Ritalin a silver bullet or black magic?
An initial concern centred on the drug’s similarity to illegal amphetamines, such as speed. As with other medical drugs, Ritalin quickly developed a parallel life as a street drug.
In 1971, a task force on drug abuse reported to the US Senate that Ritalin was causing trouble in many US cities. In Seattle, it was described as the number one drug abuse problem.

Rather than taking the drug orally, as intended, users would dissolve Ritalin and inject it. The task force also reported “children swapping their pills in the schoolyard with unfortunate effects”. In response, Ritalin’s manufacturer (now Ciba-Geigy) said they were unaware of the abuse of their product and that reclassifying the drug would stigmatise patients.
While ADHD remained primarily a North American diagnosis during the 1970s, the abuse of Ritalin in Sweden was such that the drug was banned.
Critics also highlighted Ritalin’s side effects. Although Ritalin was marketed in part on the basis that it was safe, ads warned of possible insomnia, depression, anorexia, stunted growth, bed-wetting, irritability, heart problems and hallucinations.
A 1971 study that compared Ritalin to stronger stimulants and an antipsychotic drug found that while its side effects were less frequent, they could be severe. One child experienced hallucinations that worms were crawling over him, only to return to normal when he stopped taking Ritalin.
To avoid Ritalin’s side effects, some physicians advocated taking “drug holidays” during summer and Christmas breaks. Others recommended prescribing safer stimulants, such as caffeine. Still others recommended prescribing more drugs to deal with the side effects, including growth hormones and antidepressants.
By the 1970s, Ciba-Geigy’s aggressive advertising strategy was also questioned. As well as the many ads in medical journals – some of which ran to seven pages – the company marketed directly to consumers. It organised community meetings to promote their product to parents and teachers, distributed publications widely and produced a film called “The Hyperactive Child”. Salesmen were also encouraged to target probation officers and juvenile court officers.
Although the FDA eventually restricted these direct methods, Ritalin sales continued to grow. But this very success led to new criticism about the overdiagnosis of ADHD and the overprescription of Ritalin.
As early as 1970, the Washington Post reported that 10% of students in Omaha, Nebraska were taking Ritalin and related drugs, spurring Congressional hearings. A 1976 report claimed that in Minneapolis, Minnesota, African American students were especially singled out for medication.
Prescriptions for Ritalin and other ADHD medications in the US escalated from 400,000 in 1980 to 2.6m in 1995. One reason for these increases was the broadening of the concept of ADHD.
Although ADHD had been associated with hyperactive boys, a renewed emphasis on inattention shifted the focus on girls who caused few problems in the classroom but were still struggling academically. ADHD also became understood as a lifelong, rather than a childhood, affliction, resulting in the concept of “adult ADHD”.
More recently, illicit use of Ritalin as a study aid has triggered renewed controversy. Reports describe young people “faking” ADHD symptoms to get a prescription for the drug to improve academic performance. In some cases, the drug has been a gateway to other drugs, such as cocaine and methamphetamine.
While the objections to Ritalin mounted, many patients, parents and doctors believed that its benefits outweighed the risks. Globally, the use of ADHD drugs increased as the concept of ADHD spread around the world. Iceland, not the US, now has the highest per capita rates of Ritalin use. But the crux of the matter remained: was it right to drug children to improve their behaviour and school performance?
Retirement or re-birth?
This summer, a new study threatens to cast doubt on Ritalin once again. It found that taking Ritalin for four months changed the white matter in children’s brains. In a press release, Liesbeth Reneman, a senior author on the paper said: “What our data already underscore is that the use of ADHD medications in children must be carefully considered until more is known about the long-term consequences of prescribing methylphenidate at a young age.”
(The Conversation approached Novartis – the current makers of Ritalin – for a comment on the study but did not receive a reply.)
The white matter study highlights that we don’t know enough about the long-term effects of Ritalin. Few studies have addressed this issue, despite long-term use of the drug. But even if this study’s results are replicated, would this be enough to convince people that Ritalin’s risks outweigh the promised benefits of academic and career success?
Two opposing arguments have emerged about the future of Ritalin. The first is that ADHD drugs should be made available for everyone’s benefit.
Advocates of neuroenhancement argue that we should welcome the potential improvements to our lives promised by drugs such as Ritalin. By making Ritalin more widely available, we could all benefit from improved focus and performance. We can get more done and be more effective. In Silicon Valley, for instance, people are taking nootropics, or brain-enhancing drugs, to get ahead.
But do we want to live in a world where we need neuroenhancement to be happy and successful? Advocates of neurodiversity argue that we should dismiss the concept of ADHD altogether, binning Ritalin along with it.
The term neurodiversity was coined in 1988 by Australian sociologist Judy Singer. It means that neurological differences should be recognised and respected. Rather than using drugs to change the behaviour associated with disorders, such as ADHD and autism, society should be more accommodating of neurologically diverse people.
Underlying neurodiversity is the idea that we need a wide variety of people to have successful societies. This is especially true as we try to resolve existential issues, such as climate change.
One example of neurodiversity making a difference is the teenage Swedish climate change advocate, Greta Thunberg, who has been diagnosed with ADHD and autism. It is likely that Thunberg’s unconventional approach - and her success - is partly because she thinks differently to a “neurotypical” person.
So will Ritalin play an essential part in building a neuroenhanced society? Or will greater acceptance of neurodiversity render it irrelevant? Although Ritalin may continue to play a role as a smart drug, I hope that people like Greta Thunberg convince us that we will ultimately be more successful by encouraging neurodiversity.

