Researchers have taken the first step towards designing a rapid way of identifying harmful bacteria in infections, demonstrating the potential for faster patient treatment and decreased reliance on antibiotics.
The collaborative effort, reported by journal mBio, involved scientists from many US universities and government research institutes. Led by Christopher Grim at the US Food and Drug Administration, the group aimed to identify the disease-causing genes of Aeromonas hydrophila bacteria and create a “checklist” of genes that doctors could use to spot harmful members of the species in patients.
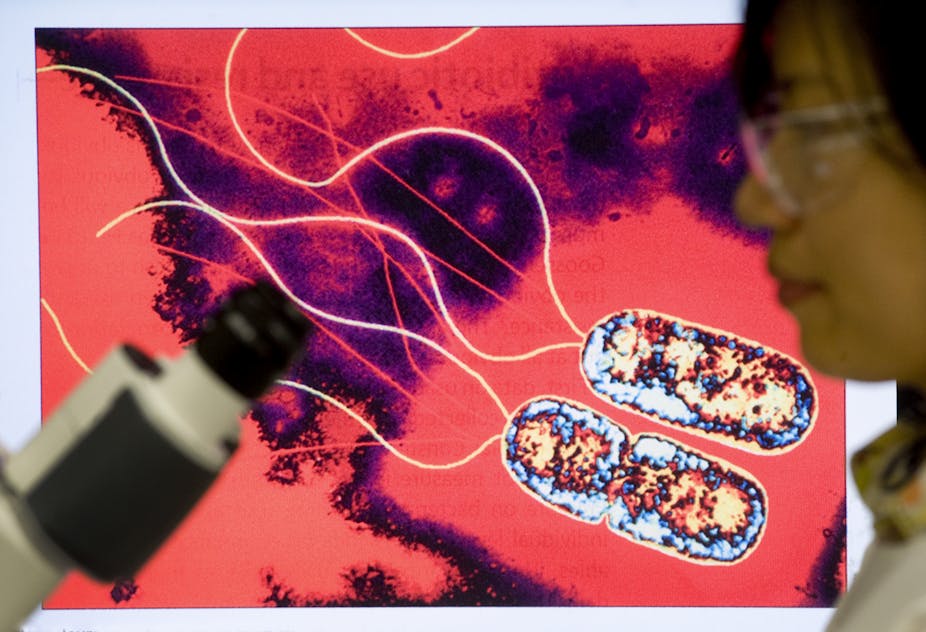
A. hydrophila is found in freshwater and estuaries worldwide, usually existing harmlessly in the environment. Occasionally, however, it can infect a human through an open wound exposed to water, or by being swallowed. Open wounds infected with A. hydrophila can result in a potentially fatal flesh-eating disease, called “necrotising fasciitis”.
The researchers investigated two strains of A. hydrophila taken from an inflamed wound. Both strains were resilient to initial antibiotic treatment, though one was more persistent and the major cause for inflammation.
They sequenced the entire genetic sequence (genome) of both types of A. hydrophila, as well as those of several close relatives. By comparing the genetic codes they identified the genes the harmful strain had that its relatives didn’t.
They then used common tests to show that a selection of the identified genes improved the bacteria’s ability to cause disease. One test investigated how effectively the bacteria destroy red blood cells, which causes inflammation. When broken up, these cells release haemoglobin - the compound that gives them their colour. The colour change this causes in a culture can then be measured.
The cause of resistance
Traditional ways of identifying bacteria of any species involve comparing bacterial growth under different conditions. This can take days, weeks or even months. During this time, patients are generally treated with broad-spectrum antibiotics that kill many bacterial species. However, as with the harmful A. hydrophila, more specific antibiotics are required to kill some pathogens.
This means that broad-spectrum antibiotics are being used unnecessarily in efforts to treat patients. Over time, this causes an increase in antibiotic resistance as bacteria evolve to defend themselves.
Joshua Shak of Emory University, a co-author of the study, believes that genetics-based diagnoses could slow the spread of antibiotic resistance. The technology’s use in identification of bacteria could allow faster turnaround on test results. This would, if selective medicines were developed, minimise reliance on broad-spectrum antibiotics, because doctors would know earlier whether specialist treatment was needed. If fewer bacteria are exposed to antibiotics then the chances of any evolving resistance are reduced.
Towards a dream
Shak acknowledges, however, that the use of genomics in diagnostics is still years from becoming commonplace. So is the development of tailored medicine. He says that, while the technology for rapid sequencing exists, analysis of the data is still a relatively slow process.
Gary Van Domselaar, a bioinformatician at the University of Manitoba, agrees with Shak. He says, “These new technologies have placed the ability to sequence biological organisms in the hands of nearly any research laboratory. The current major hurdle no longer lies in the generation of whole genome sequences, but in their analysis.”
The current limitations of data analysis are seen in this study. The A. hydrophila genome is roughly 4.7 million characters long and within it there are over 4,000 genes. The group sequenced the isolated strains’ genomes in a matter of days, yet it took years to confirm the genes involved in causing disease.
Despite this, Shak hopes that, as the genomes of more bacterial species are sequenced and analysed, further analyses will become easier and faster. This is the beginning of the dream where medicines are tailored to individual patients’ needs according to the genes of the bug causing trouble.