Many people don’t realize that their leftover tissue, blood or other samples – otherwise known as “biospecimens” – taken during a visit to the doctor or hospital might be stripped of identifying information and used in research without their consent.
This makes some people uncomfortable.
So when the federal government decided to revise its “Common Rule” regulations governing federally funded research involving humans for the first time in decades, the draft revision included a proposal to require consent for all research with biospecimens, whether they have identifying information accompanying them or not. The original regulations required a person’s consent for research with biospecimens only if they had information with them that made them identifiable.
But when the updated Common Rule was released on Jan. 18, there was no change to this part of the regulation.
Human research regulations need to keep up with major advances in technology. They also need to balance enabling scientific progress with attempting to ensure safety and privacy for human participants in research.
So why wasn’t the proposal requiring consent for all biospecimen research adopted, and how do the new regulations recognize people’s concern in what happens to pieces of themselves in the future?

Why we need human biospecimens for research
Exciting new research projects, like the Precision Medicine Initiative (PMI), aim to personalize medical interventions and therapies for things like cancer care.
But knowing how to personalize treatment requires comparing data from thousands of biospecimens to discover the relationship between genetic variation, health behaviors and medical outcomes. The PMI itself is trying to build a million-person biospecimen collection to support its research. The goal is not to just order the treatment that is best for most people – but best for you.
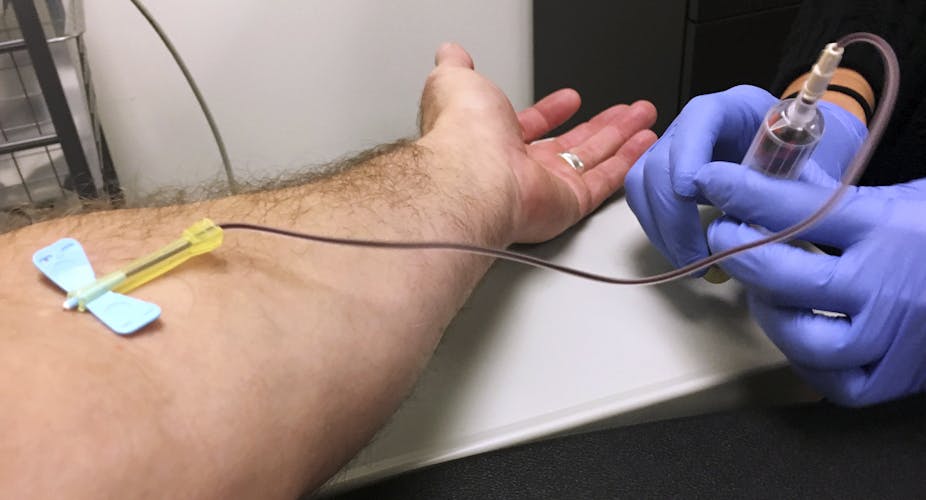
The steps required to collect those specimens are critical.
The Common Rule requires publicly funded researchers get informed consent for two kinds of work. The first is research that involves intervention or interaction with a person, like a blood draw. The second is research done with identifiable private information or identifiable biospecimens.
But if biospecimens don’t have any identifying data with them, like a name, consent is not required. Hospitals and clinics are major sources of these nonidentified biospecimens. People “donate” these samples when they, for example, have a biopsy at a hospital. These nonidentified biospecimens or information derived from them may then be made available to researchers, at the hospital and elsewhere.
Technological advances have made it possible to generate and share massive amounts of data. Large research collaborations can accomplish impressive scientific advancements, like the recent research into the genetic causes of depression. But data access can also create problems. For example, there have been cases where “nonidentifiable” information is reidentified later.
As a matter of self-determination, people are concerned about having control over their person. Generally, they want a say in what happens to their biospecimens – including what research is done with them.

These issues were raised in the 2010 book “The Immortal Life of Henrietta Lacks.” Henrietta Lacks was treated for cervical cancer at Johns Hopkins Hospital in the 1950s. Cells taken from a cervical biopsy before she died were used to create one of the most important cell lines in research. These cells, called the HeLa line, are still in use, and have lead to many scientific discoveries. But Henrietta Lacks never consented to, nor even knew, her cells were being used for research.
Research indicates that the majority of Americans are willing to donate their blood and tissue to advance research. But their willingness to do so hinges on trust. A lack of trust in scientists and scientific research is the strongest predictor of whether a person will be unwilling to donate to a biobank. People also want to know the specific kind of research being done.
As President Obama put it, “I would like to think that if somebody does a test on me or my genes…that’s mine.”
Concerns about consent for all biospecimen research
More than 2,100 commenters voiced their opinions on the proposed regulations during the recent comment period. Most discussed whether informed consent should be required for research with “nonidentified” biospecimens. And 80 percent opposed that proposal.
This change had been considered because regulators believed that the majority of participants preferred to be asked whether their biospecimen could be involved in research. But the preamble of the new rule argued that the comments on the proposal raised questions about whether that is in fact the case.
Apparently more commenters were worried that the proposal would mean fewer biospecimens would be available for research because some institutions wouldn’t (or couldn’t) implement the expensive administrative process required for getting consent. That would mean fewer people are asked for consent in the first place, and fewer biospecimens would be available for research – slowing potential advances.
In addition, some commenters were concerned that the revision could have implications for the diversity of samples available for research. Community clinics and hospitals may have faced greater affordability challenges than larger medical centers. Large medical centers are likely to collect samples from their – often homogeneous – geographic community.
Diversity is already an issue in genetic research. For instance, recent research on genetic studies found that people of African and Latin American ancestry, Hispanic people and indigenous peoples represent only 5 percent of participants involved in studies searching for associations between genes and disease.
If samples are collected only from medical centers that can afford to implement the extra consent requirement, that could potentially weaken efforts to gain samples from more diverse groups of people. In turn, that could dampen potential transformational effects of precision medicine research across race and ethnicity.
It’s worth noting, however, these comments don’t necessarily reflect how a majority of Americans feel about requiring consent for research with nonidentified biospecimens, just the majority of people commenting on the proposed rule.
Other regulations may address some concerns
While the proposal requiring consent for research with deidentified biospecimens was not adopted in the final rule, many other updates, including several regarding informed consent, were.
For example, the Common Rule updates the consent requirement for “secondary research” with identifiable data and biospecimens taken from a biobank, and not directly from a participant. These changes allow for broad consent, which would give the participant a general description of the types of research that may be conducted and information generated at the time of donation.
Another change is that the agencies that implement the Common Rule are now required to consider what an “identifiable biospecimen” means at least every four years. They also have to publish a list of what new technologies could generate “identifiable private information” from otherwise nonidentified biospecimens. This could mean that researchers might not be able to use technologies that could generate such information without consent from the subject. That could, perhaps, achieve some of the goals of the original proposal.
Also, the new rule adds to existing research informed consent disclosure requirements. One addition is that prospective subjects must be told that their deidentified biospecimens might be used for future research that they don’t specifically consent to, if that’s a possibility.
Many are still fully processing the 543-page updated Common Rule. But initial indications are that it is a thoughtful document – particularly considering potential changes in government rule-making going forward.
Where are we now?
It’s unclear what the Trump administration will do with these regulations now that they’ve been published.
The House has passed legislation that would allow Congress to disapprove or eliminate new regulations. The House Freedom Caucus (cofounded by Representative Mick Mulvaney, President Trump’s pick for budget director) had placed these research policy revisions specifically on the chopping block for Trump’s first 100 days, although that was in response to the proposed revisions.
But while regulations may be dismantled quickly, big-picture policy concerns – like public trust in science – remain to be grappled with.
Science remains critical to our national interests, and biospecimens will remain critical to science.
Whether the new administration allows these revisions to stand or pulls them, clearly there is still work to be done.