When a scrotum is empty this indicates an undescended testis. This occurs when a testis never moved down in to the scrotum as the male developed, or moves back up out of the scrotum and into the abdomen where it started.
People commonly associate this with childhood, but soon-to-be-published data suggests more untreated undescended testes in older children, and this is likely to lead to more adults with undescended testes in the community.
The journey to the scrotum
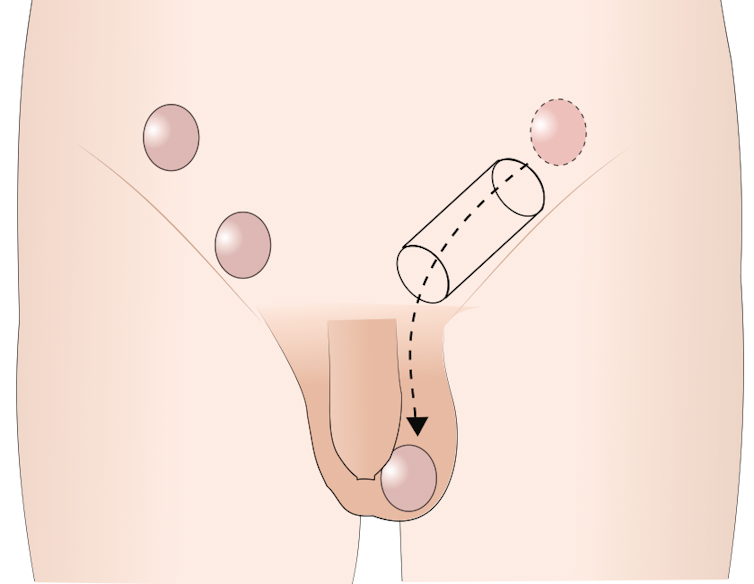
Before birth each testis (note: testis is singular; testes is plural, and testicle relates to a very small testis, such as infants. It’s colloquially, but incorrectly, used for every testes) forms on either side of the abdomen, near the kidneys, before moving down into the scrotum just before or just after birth.
At birth, 3-5% of boys have an undescended testis, with the testis located along or near this line of descent. Around half of these testes will descend into the scrotum by three months of age. This is the most common form of undescended testes.
Boys between one and ten years can also have their testis re-ascend as they grow, which is the second-most-prevalent type of undescended testis. This occurs because the testicular blood vessels, connecting it to the inside of the abdomen, do not grow as much as the distance between the groin and the scrotum. Boys who were born with undescended testis but had their testis drop by the age of three months are more likely to have their testis re-ascend.
The testis could be hiding in the abdomen, in the groin, or in the tissue around the groin. Rarely (in about 5% of cases) the testis has had interrupted blood flow earlier in life and disappeared.
Hormones are to blame for undescended testes, with different hormones being responsible for different stages of descent.
Related risks
Undescended testis are in the body and warmer (by two to three degrees Celsius) than in the scrotum. This warming prevents normal testicular development and sperm formation, leading to infertility.
Adult undescended testis describes cases that occur after puberty (post-pubertal), when the testis has been exposed to all the maturing hormones. Many boys with undescended testes find puberty causes their testis to descend. However, the increased temperature has already caused damage and poor sperm formation.
This was confirmed by a study of 52 post-pubertal men (aged 15-66) who had testicular tissue analysed following removal of an undescended testis. Only one of the 52 samples showed normal sperm formation. This shows the vast majority of post-pubertal undescended testes don’t contribute to fertility.
We treat undescended testes to maintain fertility and allow early detection of testicular cancer. A testis that was undescended from birth has a 2.75-8 times increased risk of cancer; this does not decrease after surgery and remains for a lifetime.
Testicular cancer can have no symptoms, but some men describe swelling, heaviness, change in shape or size, or a feeling of unevenness in the testes. Not having a testis in the scrotum may mask these feelings and delay a diagnosis of cancer. We do not know if testes that were once in the scrotum and then ascend over time have an increased risk of cancer or not.
Treatment
Management of post-pubertal men who present late with undescended testis is difficult. The surgical options are testicular removal (orchidectomy) or surgery to bring the testis into the scrotum (orchidopexy). Both would require a general anaesthetic. If someone is not fit for an anaesthetic, observation may be the best option.
As the majority of undescended testes cannot contribute to fertility, with increased cancer risk, testicular removal is the best option. This particularly applies if the testis has been in an undescended position for a significant number of years.
In cases with early post-pubertal surgery, or a clear history of a testis once being located in the scrotum and then ascending, surgery to bring the testis into the scrotum (orchidopexy) can be offered. Testicular implants are available in a variety of sizes to match the existing testis, and are designed to feel the same.
Undescended testis is a common issue and can persist through the teenage years into adulthood. Self-exam is a good idea, especially if you have a vague recollection of an operation when you were a child.
Yearly observation of your children, especially when they are out of nappies, is also an important take-home message. For further information please make an appointment to see your GP or urologist.

