In the ninth part of our series Health Rationing, Stephen Duckett examines the government’s decision to extend the breast cancer screening program.
As one of many pre-budget teasers, Health Minister Plibersek announced on Mother’s Day that Australia’s breast screening program will be extended to target women aged 50 to 74 instead of the current age range of 50 to 69.
There may be political benefits from this A$55 million spend, but is it a good deal?
From an economic rationality point of view, the short answer is yes. But there may be a better way to achieve greater gains.
Is breast screening worth it?
Australia’s breast screening program was announced by then-prime minister Bob Hawke in the midst of the 1990 election campaign.
But the benefits of the program haven’t been entirely political. A 2009 cost effectiveness analysis showed that the program cost A$38,302 for each year of life gained. That is a good deal compared to other health investments. Dietary counselling from a GP for people at greater than 5% risk of heart disease, for instance, costs about A$35,000 for every disability adjusted life year gained.
Although assumptions in cost effectiveness analysis of breast screening have been challenged because it doesn’t account for the the anxiety created by screening programs, this report is the best evidence we’ve got.
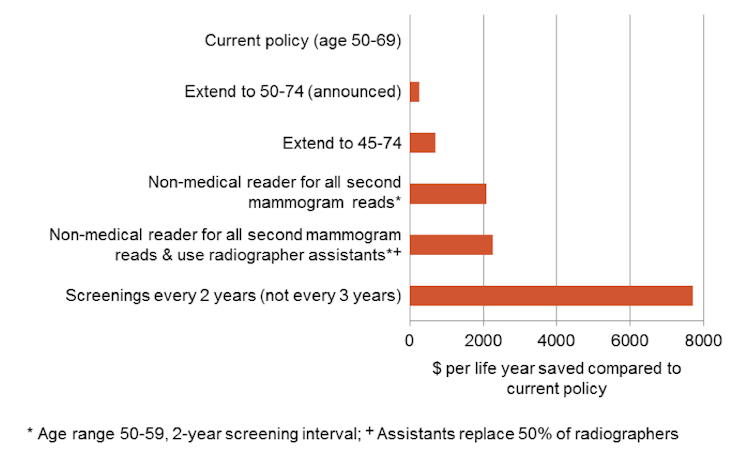
The government’s decision to extend the age range of women eligible can be seen as economically reasonable because of the reduced cost per year of life gained. Economic rationality and rationing is not a euphemism for budget cutting. Based on current evidence, expanding these services is the right thing to do.
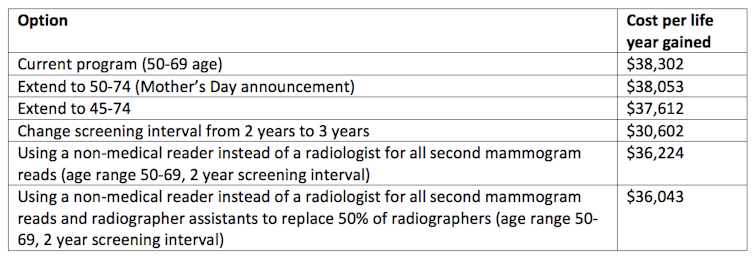
But here’s the rub. Extending the age range down to 45 and up to 74 is even better on cost-effectiveness criteria. With that policy, the cost per year of life gained from screening would be A$37,612 compared to the current A$38,302 – a 2% improvement. Small, yes, but important in the overall scheme of things.
Cost effectiveness isn’t the only relevant criterion, though, even for the econocrat. Extending the age range both upward and downward would cost much more money than just an upward change. In tight budgetary times the larger extension, although economically worthwhile, may have been a budget step too far.
Roads not taken
Yet, if increasing the age range were combined with efforts to cut the cost of screening, we might be able afford the best of both worlds: even more breast cancer screening without hurting the budget bottom line. Cost-effective expansions and budget integrity might both have been feasible.
The 2009 cost effectiveness report also examined changes to current practice and identified several ways to save money, while still saving lives. Increasing the screening interval from two to three years is certainly cost effective and would save significantly on budget outlays. The government could easily afford an age range expansion in both directions if that change were implemented.
Changes in who can conduct and read mammograms are also cost effective. Currently, every mammogram is examined independently by two radiologists. One cheaper and more cost-effective option assessed was to have the second reading done by a specially trained reader. Changes in who takes the mammograms – a radiographer assistant rather than a radiographer – would also lower costs.
There is still some controversy about breast screening and new evidence is becoming available every day. The 2009 cost-effectiveness study was a “modelling” study, not an assessment in the real world. In contrast to the Australian approach of simply announcing an expansion of breast screening, a similar expansion in the English National Health Service was accompanied by a randomised controlled trial to allow a full evaluation of the new policy.
It’s puzzling why a similar strategy was not followed here, especially in the light of recent calls for more health services research in Australia to contribute to policy development.
Burgeoning health outlays
Health expenditure is rising rapidly. Budget setting is about priority setting (the soft way to say “rationing”). But the rationing discussion should follow, not replace or precede, the efficiency discussion. The extra money to expand screening to wider age groups could have been offset completely by improved efficiency.
Current policy settings in breast screening “ration” the public program to women aged 50-69. The government has just announced a new “rationing” regime, to target women 50-74, and this indeed is a rational expansion, as far as it goes.
But the real rationing question is: in hard economic times, why aren’t we pursuing other breast-screening initiatives – such as changing the screening interval and using a different mix of health professionals – that are more economically rational and save more money?
This is the ninth part of our series Health Rationing. Click on the links below to read the other instalments:
Part one: Tough choices: how to rein in Australia’s rising health bill
Part two: Explainer: what is health rationing?
Part three: A conversation that promises savings worth dying for
Part four: Phase out GP consultation fees for a better Medicare
Part five: Focus on prevention to control the growing health budget
Part six: Health funding under the microscope – but what should we pay for?
Part seven: Comparing apples, pears and hips: health rationing at work
Part eight: Who gets a piece of the pie? Spending the health budget fairly

