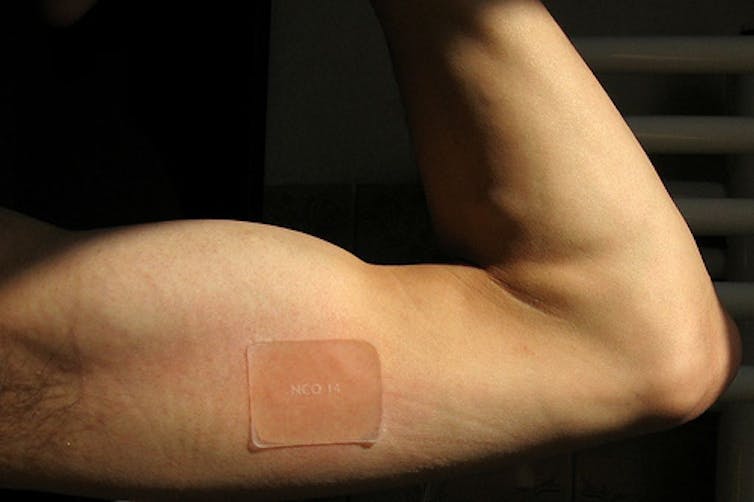
Pharmaceutical companies have aggressively promoted nicotine replacement patches, chewing gums, inhalers and nasal sprays as effective tools to improve smokers’ chances of quitting for more than 20 years. But two studies published this month add to a small but growing body of evidence that smokers don’t need to resort to pharmaceuticals to quit.
Current guidelines for medical advice and hospital-based quit programs in the United States recommend smokers are treated with, or are at least offered, an over-the-counter nicotine replacement therapy (NRT) or prescription medicine (excluding pregnant women and some other small, specific population groups). These recommendations go well beyond the available evidence about the efficacy of cessation medications.
Researchers at the Harvard School of Public Health and the University of Massachusetts recently studied the attempts of 787 Massachusetts smokers to quit and found the use of NRT had no effect on on their success.
In the second study, published in the prestigious Annual Review of Public Health, lead author John Pierce and his colleagues argued that rather than helping smokers quit, the widespread marketing of nicotine replacement therapy had reduced expectations about how difficult it was to quit.
The biggest casualty from this overconfidence in pharmaceuticals has been the neglect of unassisted, or cold turkey, quitting. Pierce notes examples of cessation policy that actively discourage unassisted quitting “despite the documented high success of this approach”.
To assess how people stop smoking, my colleague Simon Chapman and I collated and analysed data on success rates of different methods. We found that the majority of ex-smokers had managed to break their habit without resorting to pharmaceutical products – and argued that this message should be communicated to smokers.
Perhaps surprisingly, our 2010 paper attracted widespread criticism from within the tobacco control community. Much of this disconnect comes down to the chasm between clinical trial results and success rates in “real world” situations. While randomised trials of nicotine replacement therapies report success rates as high as as 50%, widespread use of these products over the past two decades has not improved successful quit rates at the population level.
Participants in tightly-controlled clinical trials are selected according to restrictive selection guidelines and receive free medication, health care and counselling; all of which contribute to inflated success rates.
The role of the pharmaceutical industry is key factor in this research. A 2007 review of selected controlled trials of NRT found more than half (51%) of industry-funded trials reported significant cessation effects, whereas only 22% of non-industry funded trials reported the same benefits.
Using favourable trial results, pharmaceutical corporations have aggressively marketed the idea that smokers won’t be able to quit without using NRT, or other prescription medications such as bupropion (Zyban, Prexaton) and varenicline (Champix).
In Australia, industry campaigns are bolstered by the federal government’s National Tobacco Campaign which promotes the use of NRT prior to a quit attempt. But despite two decades of such promotion, between two-thirds and three-quarters of former smokers have quit without using any sort of medication.

Time to re-think policy
When Australia’s Department of Health and Ageing evaluates drug funding applications, the most important factor it considers is the results of clinical trials. So it’s not surprising the government decided last year to subsidise nicotine replacement by placing it on Australia’s Pharmaceutical Benefits Schedule, at a cost of more than A$9m in 2011.
Nicotine replacement therapy undoubtedly works for some smokers and in these cases is the appropriate course of action. But the use of public funds to provide such therapies to the population at large is of questionable value, especially if funds are diverted from evidence-based, population-level programs.
In the past two decades Australia has enacted legislative restrictions on public smoking, bans on tobacco advertising and promotion, and regular tax increases on tobacco products. And it’s these initiatives that are responsible for driving our national smoking rate down to 17%, one of the lowest in the world.
This is where future anti-tobacco funding and public policy efforts should be directed.

