There have been national, state and local campaigns to “Close the Gap” in Australia. Despite this, considerable health gaps still exist between Indigenous and non-Indigenous people.
Musculoskeletal conditions are an area of health where there is a significant difference between Indigenous and non-Indigenous people. Although Indigenous people experience musculoskeletal conditions more, their access to high-quality and culturally informed support remains low.
Musculoskeletal conditions can have a considerable effect on people’s lives. Such conditions can affect a person’s ability to walk, complete simple tasks at home without help, and participate in sports or work.
Government health organisations need to provide better support for Indigenous people suffering from these conditions by encouraging culturally safe community-based care.
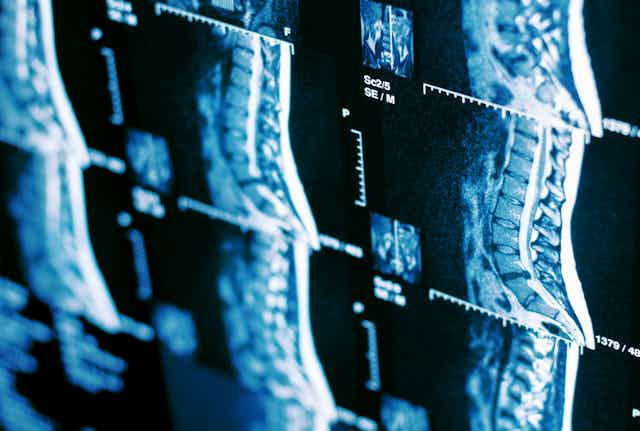
What are musculoskeletal conditions?
Musculoskeletal conditions include disorders that affect the bones, muscles and joints such as back pain and osteoarthritis. They affect approximately one in three Australians.
Internationally, low back pain is the leading cause of disability, and osteoarthritis is the leading cause of physical activity limitation. Both of these ailments are more common in Indigenous people, who are 20-50% more likely to have osteoarthritis and 10% more likely to report current back pain than the non-Indigenous population in Australia.
Musculoskeletal conditions have also been shown to contribute to the development of chronic diseases such as diabetes and cardiovascular disease. With 46% of Australia’s Indigenous population having at least one chronic condition, this may lead to even higher rates of chronic diseases.
Many Indigenous people resign themselves to being in pain and living with their condition. The social impact of living with these conditions is important to consider. For some First Nations people, it has the potential to restrict participation in activities of cultural significance and minimising connection with family and Country.
For example, the ability to care for and connect with extended family, attend community and family gatherings and enjoy activities on Country. These limitations often have considerable emotional effects on individuals, leading to feelings of anger, depression and fear.
Community-based care is needed
Indigenous people’s access to health-care services to manage pain is half the expected rate compared to non-Indigenous people. Part of the reason for lower health care access is due to negative experiences with health-care services due to discriminatory attitudes toward pain from health-care providers. Unfortunately this is a common occurrence for Indigenous people. More than half (53%) of all Indigenous people have experienced racism when when seeking health care.
Ways to increase Indigenous peoples’ access to health services is for them to have better support with self-managing their condition. In addition, community-based approaches to health care would provide a safer space for these patients. The Indigenous Australians’ Health Programme and other funding bodies must work with communities, clinicians, and researchers to deliver programs addressing musculoskeletal conditions and chronic diseases. These programs need to ensure local communities are at their centre and cultural safety for participants is a priority. Such programs could be led by community-based allied health clinicians, but should include a range of health professionals to ensure optimal care is provided that addresses all factors related to musculoskeletal conditions.
Health care needs to include cultural safety
A whole of system approach is required to improve access to health care for Indigenous people in Australia. National, state, and local services must work together to ensure culturally safe care is provided, placing Indigenous clients and local communities at its core. This shift will likely require changes in how clinicians deliver care, how the services organise care, and how the health-care system supports this care.
Ineffective communication is often sighted as a barrier to care for Indigenous people. This is why clinicians building connections and rapport with the Indigenous community they are treating is important. Undertaking training in cultural safety and effective communication strategies is essential to assist clinicians in providing optimal care.
To improve health services, programs providing care for musculoskeletal conditions should aim to partner with Aboriginal Community Controlled Health Organisations and ensure Indigenous people are trained and employed as part of the team. The health system should also ensure policies prioritise these employment opportunities as well as the importance of providing culturally safe care and working with local Indigenous communities.
A person’s musculoskeletal pain and the presence of chronic diseases are often intertwined. We must develop community-based models of care to address these conditions in Indigenous people, and ensure culturally safe care is being provided. These changes will require ongoing training for health-care staff.
The fundamental shift is the inclusion of local Indigenous communities in all health care initiatives. These improvements will help ensure Indigenous people have the opportunity to self-manage their musculoskeletal pain, general health and well being.