It’s been ten years since bluetongue virus (BTV) arrived in Britain for the very first time. With UK conditions mirroring those in Holland where the virus was already circulating, its arrival had been widely anticipated – a case of when, not if.
BTV causes a disease called bluetongue in cattle and sheep (although it is mostly sheep that are affected). The clinical signs for bluetongue can range in severity, from little or no sign of disease through to death.
The virus initially parachuted into northern Europe in the autumn of 2006 and seeded itself across wide areas in countries such as Germany and the Netherlands. The outbreak itself was unprecedented; BTV is normally a disease of the warm tropics and subtropics, and had never before been seen as far north in Europe as in 2006.
The strain that arrived – BTV8 – turned out to be particularly severe, with cows as well as sheep suffering high levels of infection and mortality. This was also final proof that the species of Culicoides midge present in northern Europe were just as able to transmit the virus as those found in tropical parts of the world.
BTV survived the European winter and emerged the following year, becoming one of the largest recorded outbreaks. All it took was the wind blowing in the right direction to carry infected midges across the Channel and BTV was able to enter the UK.
Sequencing foot and mouth disease
Throughout the BTV8 outbreak, molecular assays – tests that detect and characterise the genetic material (the genome) of the virus – played a key role. It can take days to isolate a virus in the lab using traditional approaches, whereas molecular assays can provide a result within hours.
BTV comes in at least 28 different forms, called serotypes, which to the immune system all appear different. Knowing which serotype is present is critical for choosing which vaccine to use (or develop if one doesn’t exist). In the case of BTV8, molecular assays were also the first to determine the serotype of the virus.
BTV landed in the UK just as an outbreak of arguably the most feared disease of livestock – foot and mouth disease (FMD) – was in its final stages. The FMD outbreak was first reported on a cattle farm in Surrey on August 2 2007, and soon spread to neighbouring farms.

Unlike the UK outbreak of FMD in the UK in 2001, molecular methods of virus diagnosis and characterisation came to the fore in 2007. A form of reverse-transcriptase polymerase chain reaction (RT-PCR) known as real-time RT-PCR was used extensively in the 2007 outbreak of FMD.
Real-time RT-PCR is capable of amplifying and detecting the foot and mouth virus (FMDV) genome, if it is present during the amplification stage, achieving a result within a matter of hours, as opposed to days – which meant that the outbreak could be controlled with greater precision and speed.
Historically, virus genomes were sequenced after an outbreak to assess how the virus had spread and understand where it had come from. The foot and mouth outbreak of 2007 represents the dawn of generating whole genome sequences in real time, during an outbreak, to inform decisions.
By characterising the complete genome it was possible not only to determine the strain of virus – in this case a variant of the virus called “type O” – but also track its progress as cases arose.
Genomes are comprised of individual units - nucleotides - linked together to form a code. Previous work had shown that around four nucleotides (out of around 8,400 which make up the genome) change as the virus moves from farm to farm. So when a gap of nine changes was found, this meant there were as yet unidentified infected farms still to be discovered.
Molecular epidemiology was not new at this point. Studies have been performed on many viruses, allowing us insights into where viruses invade from and the driving forces behind outbreak dynamics. For example, a study in Vietnam showed that Dengue virus circulates in the south, but periodically moves north via human movement.
Similarly, scientists at Glasgow University were able to uncover how and when hepatitis C virus entered and spread in Scotland, as well as identifying hotspots of transmission. However, using genome sequencing during an outbreak was comparatively new.
Fighting Ebola
Seven years later, real-time sequencing of viral genomes during an outbreak finally came to prominence during the outbreak of the Ebola virus in West Africa. Until 2014, the epidemiology of Ebola outbreaks, as with many other viruses, was still based around traditional methods of tracing contacts and trying to work out where someone had become infected – and then trying to work out where the infection may be heading.
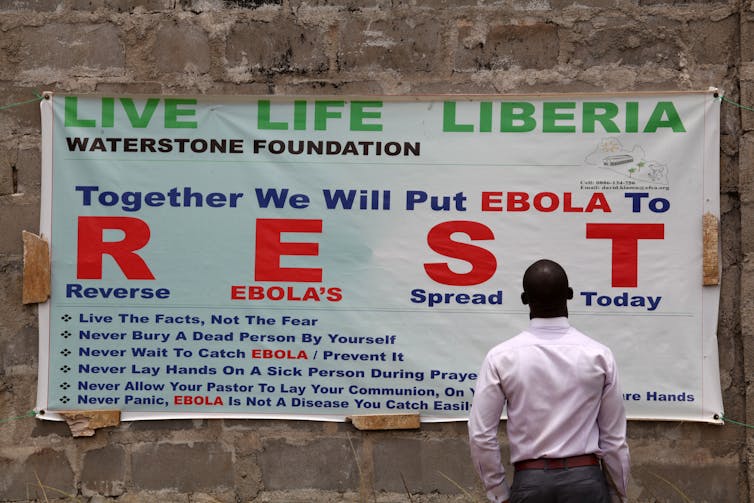
This “rubber boots” approach is still invaluable and essential for investigating and controlling outbreaks. Nevertheless, technology has reached a stage now where molecular approaches – and in particular genome sequencing – can be performed sufficiently rapidly in the field and can inform future decisions.
In the case of the Ebola virus, sequencing the virus in samples in real time quickly established that there were two lineages of Ebola in Guinea. Setting up a sequencing facility in Sierra Leone in turn revealed at least nine lineages circulating there.
By associating a sample with a particular lineage it was possible to resolve chains of transmission to a level of detail otherwise unachievable. The same group has now taken the field approach to the Zika virus outbreak in South America, again with the aim of informing epidemiology via sequencing.
Real-time sequencing of viruses is not an alternative to traditional epidemiology; it merely adds more detail. Ten years on from the foot and mouth outbreak of 2007, molecular methods can now reveal crucial details that contribute to the tracking, control and, ultimately, halting of infectious disease outbreaks.

