In rural sub-Saharan Africa, a child who wants to succeed in school faces an uphill struggle. Families often lack the income they need to pay school fees and those who are fortunate enough to attend may still lack supplies or proper nutrition. To add to this burden, children are often the favoured host for infections that hinder their growth, development, and in many cases, survival.
These infections, called “neglected tropical diseases” (NTDs), infect a billion people globally. They most commonly occur in tropical and sub-tropical countries and the people they affect are predominantly low income, surviving on less than US$2 a day. By keeping those infected with NTDs chronically ill, these infections propagate a vicious cycle that holds back the world’s poorest populations from ever rising in health or wealth.
Meet the diseases
While NTDs are classified differently by organisations, they typically include at least 13 different infections caused by parasitic worms, bacteria, protozoans, and viruses. Cumulatively, they cause 534,000 deaths a year. This is far less than the death toll of diseases like HIV/AIDS and malaria. But NTDs reduce the capacity of those infected, and in areas that are also heavily burdened by malaria and HIV/AIDS, NTDs can accelerate the progression of these killer diseases or exacerbate their symptoms.
In school-aged children, parasitic worm infections diminish focus and cause physical and intellectual stunting. In adults, these same infections have been associated with wage reductions of up to 20%, directly resulting from fatigue and cognitive sluggishness.
Other NTDs, like leprosy, onchocerciasis (river blindness) and leishmaniasis (the most severe form, kala-azar, is second only to malaria in deaths by parasitic infection) cause deformations that can physically disable the infected from performing household or community duties.
But because the burden of these diseases are subtle and difficult to consistently attribute to infection, their effect on people and their livelihoods is frequently under-represented.
Disability life adjusted years are often used to calculate the burden of diseases by combining the total number of years lost as a result of ill-health, disability, or early death. In disability life adjusted years, the burden of worm NTDs alone is as significant as malaria and tuberculosis combined, despite NTDs less frequently causing death.
Counting the cost
Between 1975 and 2005, a few effective drugs for the treatment of NTDs were produced, but the development of new drugs has since come to a near total standstill. This is in part because the pharmaceutical industry cannot recover the costs of drug development from patients who often cannot afford to pay for treatment.
And the drugs are generally cheap – a one year treatment for schistosomiasis (bilharzia) infection costs less than 50 US cents per person. In developed countries, where NTD infections are rare and usually result from travel to high transmission countries, these drugs are readily accessible. This isn’t the case in developing countries. Challenges in drug availability result from lack of infrastructure, government resources, and in some cases, like in the Middle East and Sub-Saharan Africa, political instability.
The issue is compounded by the fact that all low income countries are affected by multiple NTDs at the same time. This makes it even more difficult to control or prevent escalations in disease.
In recent years, concerns about these diseases developing resistance to commercially available drugs have also surfaced and there is evidence that some NTDs are already becoming resistant. For example, effectiveness of antimonal drug treatment for leishmania in one north Indian state has dropped to less than 50%, which suggests resistance. Another drug praziquantel was developed in the 1970s and is drug of choice for treating schistosomiasis. But the parasitic flatworms that cause the disease also appear to be developing resistance in both the lab and field.
Resistance is especially concerning because of the lack of new drugs – for many NTDs there are no alternatives under development. Instead, the recent focus of disease research is almost exclusively associated with illnesses that affect wealthy countries, like cardiovascular diseases and cancer.
In 2008, of the US$100 billion in funds contributed globally to pharmaceutical research and development, only 3.1% was dedicated to NTDs. This funding was also heavily skewed towards the “big three”: HIV/AIDS, malaria, and tuberculosis.
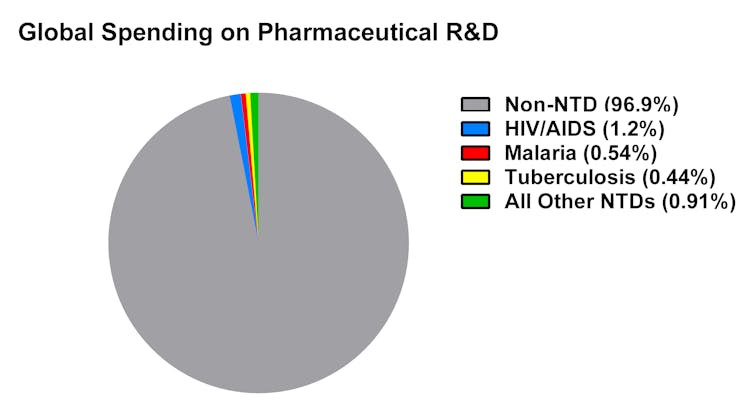
NTDs that were uncommon outside of impoverished tropical areas but caused equally devastating effects (measured in disability adjusted life years) received incredibly lean funding – less than 6% of total NTD revenue.
Outside charity’s remit
The majority of funding for NTDs comes from charitable donations. With little or no funding coming from the pharmaceutical industry, the funds that are available for combating NTDs tend to go towards basic research. Drug or vaccine development is often out of the scope of donor involvement. Inadequate, piecemeal donations with no clear plan of spending priorities typifies NTD funding. It also makes the chances of new, cost-effective drugs or vaccines for many NTDs implausible.
The future of treatment is bleak without additional support from governments and pharmaceuticals. But there is promise in prevention. Many NTDs are a result of limited education and poor sanitation. Soil-transmitted worms, for example, can be avoided through proper footwear (some worms are capable of piercing through the soles of feet), and by using latrines that separate infected stool from areas that people contact.
Preventive measures, which include education and improving public health infrastructure ,can go a long way in affected countries. Most importantly, they offer an opportunity to unburden the world’s poorest people from the diseases that challenge their health and survival – and perhaps then, a chance to thrive.

