Yoshinori Ohsumi was awarded the 2016 Nobel Prize for Physiology or Medicine on Oct. 3 “for his discoveries of the mechanisms for autophagy”, which is how cells “recycle” their contents. Autophagy is a quality control mechanism that destroys invading pathogens, such as bacteria and viruses, detoxifies harmful materials and recycles large proteins into their individual building blocks, called amino acids. This lets the cell clear out harmful materials.
Autophagy is essential for the life and health of the cell. Defects in autophagy can lead to a host of diseases. In fact, autophagy defects are a common denominator in neurodengerative diseases, including Parkinson’s and Alzheimer’s.

Ohsumi identified key genes and molecules behind autophagy. In so doing, he shifted scientific paradigms about cellular quality control. He opened the gate for researchers like me to understand how defects in autophagy are associated with neurological diseases.
In fact, my lab at Georgetown University is exploring FDA-approved cancer drugs that are known to activate autophagy as potential treatments for Parkinson’s and Alzhiemer’s disease.
Autophagy defects and neurodegenerative disease
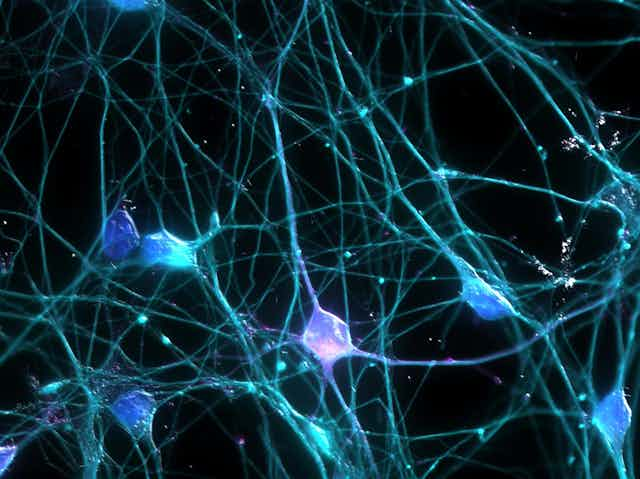
In neurodegenerative diseases, toxic proteins accumulate within brain cells called neurons.
Neurons are irreplaceable. They must continue to recycle proteins and break them down into small amino acids to avoid a toxic buildup of abnormally large proteins. That is what autophagy lets them do.
The process works by sequestering unwanted proteins into pipelines called “autophagosomes.” Then they dump those proteins into a part of the cell called a “lysosome,” where they are recycled. When this process doesn’t work properly, harmful proteins can accumulate.
Defects in autophagy are a common factor in neurodegenerative diseases regardless of aging, gene mutations, environmental toxins, infections and abnormal proteins.
When my lab examined postmortem Alzheimer’s and Parkinson’s brains, we found that the molecular steps of autophagy are broken, leading to accumulation of the toxic proteins.
So if we can find a way to activate autophagy or repair the molecular cascade that kicks it off, cells could once again clear out harmful proteins. Work from my lab suggests that certain cancer drugs may actually do this.
Using cancer drugs to jump start autophagy
My lab has demonstrated that a number of cancer drugs can trigger the molecular cascade that kicks off the whole process.
Specifically, these drugs activate a protein called “parkin,” which is involved in the autophagy process. So activating parkin can activate autophagy, thus clearing neurotoxic proteins.

Keep in mind that cancer drugs work by killing cancer cells and can also be toxic to other cells. So our first step was to find out how these drugs worked in cancer cells and neurons. Our initial observation in cell culture models was stunning: Cultured cancer cells died while cultured neurons survived after treatment with several autophagy-stimulating cancer drugs.
Next we introduced toxic proteins into cultured neuronal cells and treated them with several cancer drugs that activate autophagy and destroy tumors. The cells treated with these drugs survived and cleared their toxic proteins, while untreated cells died.
A cellular balancing act
Activating autophagy is a double-edged sword. One the one hand, the process clears toxic or infectious materials from cells. On the other hand, if the autophagy process goes beyond “recycling” and clearing out proteins, it can start to destroy the cell, leading to cell death.
This means that autophagy must be carefully manipulated to avoid the death of nonrenewable and irreplaceable neurons.
When we tested these cancer drugs in animal models to see if we could trigger autophagy without killing irreplaceable neurons, we used very low concentrations of autopahgy-inducing drugs. Autophagy was activated in neurons for only three to four hours a day, just enough to clear the toxic proteins, but stopping short of causing cell death.
Later we tested these drugs in animal models of Alzheimer’s and Parkinson’s disease. We found that they activate autophagy, clear toxic proteins and reverse cognitive and motor defects.
Now we are researching several other drugs known to enter the brain at low concentrations and induce autophagy in models of dementia and Parkinsonism.
Might it work in humans?
Based on our research in cells and animals, we performed our first clinical study to demonstrate the safety of the cancer drug nilotinib in patients with Parkinson’s disease with dementia and Lewy body dementia.
The results exceeded our expectations, providing both molecular and clinical evidence that nilotinib may benefit these patients.
Soon we will begin recruiting participants for two phase II trials to test data safety and efficacy. One trial will focus on Parkinson’s and the other on Alzheimer’s. We are also preparing a phase IIa clinical study with nilotinib in Lou Gehrig’s disease and bosutinib in a phase I study. Another cancer drug, Pazopanib, will be next in our pipeline.
These clinical studies owe much to our understanding of the basic biological mechanisms of autopahgy described by Dr. Ohsumi. His work has brought biology and medicine closer to finding treatments for chronic and deadly diseases.