An expensive IVF technique, routinely offered in fertility clinics around the world, offers no extra benefits to standard IVF in the vast majority of cases, our new research shows.
The technique, known as intracytoplasmic sperm injection or ICSI, was developed to help couples where the man has a low sperm count. But it is now the main fertilisation method clinics use in Australia and New Zealand, even when sperm counts are normal.
In an article published today in The Lancet we show that when there’s a normal sperm count, ICSI does not improve the chance of a baby when compared with standard IVF. So why do clinics routinely offer it?
Read more: Considering using IVF to have a baby? Here's what you need to know
What is ICSI?
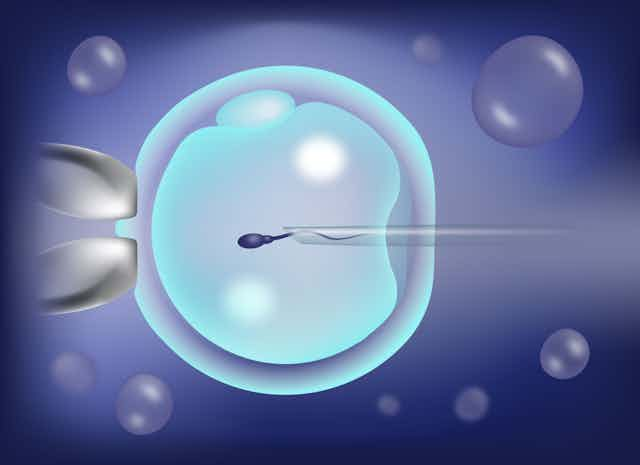
In IVF, several thousand sperm compete to be the one to fertilise an egg. However, for the small percentage of couples with what doctors call severe male-factor infertility — for instance, where there is a very low sperm count or the sperm doesn’t look or move normally — IVF is not an option.
In 1992, ICSI was introduced, where a single sperm was injected into the egg using a glass needle. This allowed the expansion of IVF to people where low sperm counts or poor sperm quality was an issue.
Its introduction across the world has helped thousands of couples have biologically related children, who otherwise would have needed donor sperm or remained childless.

How common is it?
ICSI was expected to be used only where male infertility was an issue, but over time it has become the most used method of fertilisation even when it isn’t.
In the United States, between 1996 and 2012, ICSI use increased from 15% to 67% of couples where the male has a normal sperm count; in Europe about 70% of cycles use ICSI.
In Australia around 60% of cycles used ICSI in 2018. This is even though only 30% of infertile couples have male infertility and 15% severe male infertility.
Clinics in Australia use ICSI to different extents. For instance, in Victoria in 2019-20, ICSI was used between 34% and 89% of the time, depending on the clinic.
Read more: Sperm: why these secretive swimmers are the key to the future of fertility – and contraception
What we did and what we found
Today we report, with our collaborators in Vietnam, the results of a large study in which more than 1,000 infertile couples with a normal sperm count were randomly allocated to ICSI or IVF. We found couples in either group were just as likely to have a baby.
This adds to evidence from other large observational studies in as many as 15,000 women that the widespread use of the more expensive and technically demanding ICSI does not offer any benefit to couples where the man has a normal sperm count.
Excellent clinics internationally and in Australia perform ICSI in fewer than 35% of their treatments, while achieving success rates equal to or better than clinics using ICSI more commonly.
Read more: Fertility miracle or fake news? Understanding which IVF 'add-ons' really work
How did ICSI become so popular?
There are a growing number of fertility treatments that aren’t backed by reasonable evidence.
Some are relatively cheap, such as vitamins and antioxidants. Others are invasive or expensive. These include endometrial scratching (where the lining of the uterus is scraped with a thin tube, which is said to improve the chance of an embryo implanting), video microscopy of embryos, and pre-implantation genetic diagnosis for potential chromosome abnormalities (where an embryo is tested for genetic disease before being implanted).
In fact, ICSI is about A$500 more expensive than standard IVF, although costs vary between clinics, and some costs can be claimed on Medicare under specific circumstances.
So why are these so-called “add-ons” or “adjuvants” so common?
Fertility treatment, especially IVF and ICSI, is overwhelmingly practised in the private sector in Australia and New Zealand. It is strongly marketed to the public and promoted in social media by individual doctors, clinics and corporations. Doctors and clinics also compete for patients, often offering unproven therapies.
Read more: The business of IVF: how human eggs went from simple cells to a valuable commodity
Couples may overlook a doctor seeking to practise fertility medicine based solely on evidence, and instead find a nearby clinic or doctor prepared to offer add-ons they believe will improve their chance of a baby.
In the case of ICSI, doctors may recommend it for fear of patients’ reactions if the eggs don’t fertilise, even if ICSI doesn’t improve the ultimate chance of a baby for those with a normal sperm count.
What can we do about it?
Infertility is distressing and, in most cases, can be easily treated with good advice, simple drugs and, if needed, quality assisted reproductive procedures such as IVF.
However, unrestrained, unnecessary use of ICSI is a salutary example of why we need to act on widely accepted evidence.
Until now, the fertility industry has promoted self-regulation over being made to follow government-imposed, evidence-based guidelines of which fertility treatments are needed. And there’s a growing concern the industry is not doing enough to combat unproven and expensive treatments.
Couples with infertility belong to a very vulnerable group who will do almost anything to achieve a pregnancy. They deserve our dedicated care and evidence-based treatment.