Several bacteria are already linked to human cancers, and new evidence points towards a link between Escherichia coli (E. coli) and an increased risk of bowel cancer. Luckily there are things we can do to limit the risk posed by bacteria.
The links between bacteria and cancer have been studied for a long time. The connection was first publicised in the 19th century when Rudolf Virchow suggested that cancer may result from inflammation triggered by infections. Soon after, well known scientists Robert Koch and Louis Pasteur found bacteria in tumours.
Bacterial infections nearly always cause inflammation, which occurs when our immune system recognises an infection. Immune responses often involve the release of molecules called cytokines that help to cause inflammation. Short-term stimulation of inflammatory cytokines is good and helps fight infections, but chronic stimulation can contribute to cancer development. Inflammation is a key feature that researchers are interested in, and new knowledge could help us to reduce our cancer risk.
Many bacteria have been linked to cancer via inflammation – Helicobacter pylori and stomach cancer, Salmonella typhi and gallbladder cancer, Streptococcus bovis and bowel cancer. Considering what we know now, this isn’t all that surprising.
Trillions of bacteria live in your digestive system, with hundreds of different species of bacteria living in your bowel alone. Bowel cancers are responsible for the fourth highest number of cancer-related deaths worldwide, and yet only a small percentage of bowel cancers are linked to genetic risk. The majority of new cases occur somewhat randomly (sporadic cancers) or related to inflammatory bowel disease (IBD-associated cancers).
This is where bacteria become important.
Most of the bacteria that live in your bowel are relatively harmless. In fact, they help with digestion, produce vital vitamins and help to repair damaged cells. But some bacteria are harmful. We are normally protected from harmful bacteria by our immune system and by other bacteria. Unfortunately, lifestyle factors such as high-fat diets, smoking and stress can cause chronic inflammation. Under these conditions the good bacteria struggle to survive, while some harmful, or “pathogenic”, bacteria thrive and multiply. High numbers of pathogenic bacteria means higher risk of a dangerous infection.
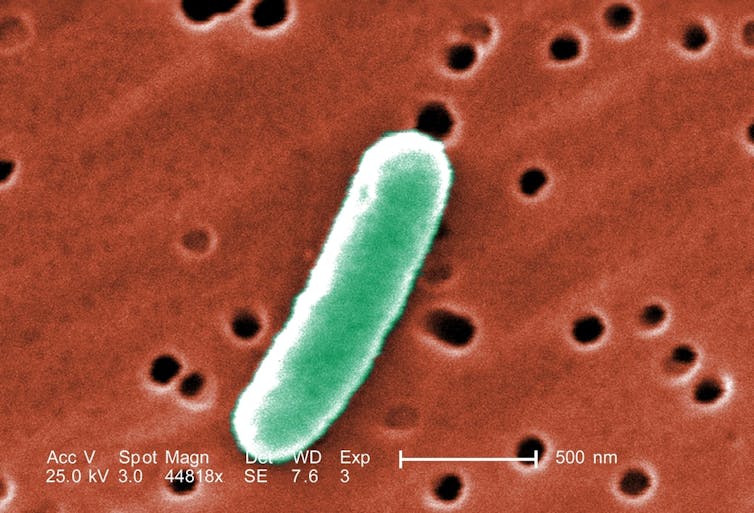
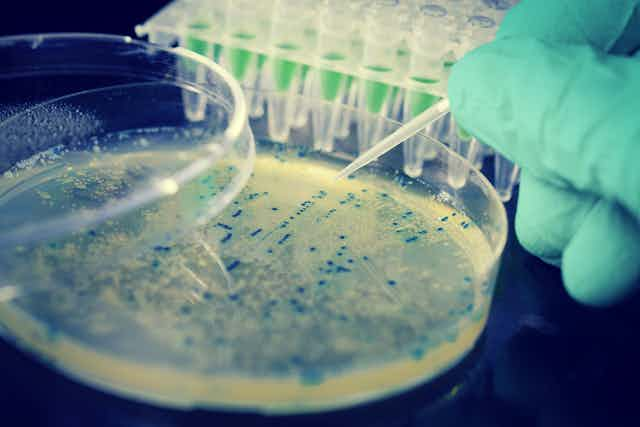
High numbers of E. coli have been found under inflammatory conditions. Some types of E. coli can be beneficial and used to treat disease; these can be found in most healthy people. However, inflammation increases the number of pathogenic E. coli and this can lead to disease. Patients with inflammatory bowel disease and bowel cancers have been found with huge numbers of pathogenic E. coli living inside tumours. That’s because these E. coli can stick to and invade the cells lining our bowels and replicate inside them. To make things worse, these E. coli are capable of producing a toxic substance called colibactin that damages the DNA of bowel cells making them cancerous, and can help cancers to spread.
Damage control
Luckily, there are things we can do to limit the risk posed by pathogenic E. coli and other pathogens.
Smoking, stress and high-fat diets are lifestyle factors that contribute to increased risk. Changing to a healthier, high-fibre diet can help to limit your bowel cancer risk and the impact of pathogenic bacteria. This is known as a “prebiotic” effect where dietary fibres produce a substance called butyrate. Butyrate has natural anti-inflammatory properties and can help replenish probiotic bacteria too.
Also, dietary fibres from plantains, bananas and broccoli can block harmful bacteria from sticking to your gut cells and promote their passage out of the gut. This is known as a “contrabiotic” effect and was recently shown to be effective against bacteria such as E. coli and Salmonella.
Vitamin D has been shown to help kill pathogenic bacteria, particularly E. coli, even when they are already inside our cells. Vitamin D deficiency is now associated with colon cancer, so maintaining healthy levels of vitamin D could further reduce your risk.
Foods such as almonds, red onions and chives are high in molecules known as flavonoids that have antibacterial properties and could help limit the effects of pathogenic bacteria.
Regular exercise helps maintain a normal bacterial diversity in the gut and could reduce your risk of bowel cancer by up to 50%.
Anti-inflammatory drugs such as aspirin have been shown to reduce the risk of bowel cancer. It is highly possible that future studies could find anti-inflammatory drugs reduce the inflammation caused by infections and hence your bowel cancer risk.
In the coming years we are likely to see both drug-based and natural treatments that specifically target E. coli and other bacteria associated with bowel cancer risk.
With researchers looking for more of these types of answers we are being enabled to fight bowel cancer in different ways. Therefore, it is becoming more necessary for us to be proactive and increase our awareness of the impact we can have before cancers can even develop.