There are many examples in history of drugs that have been repurposed for different diseases. One such drug is chloroquine, which was and is still used for malarial treatment. It has been repurposed as an anti-inflammatory, anti-diabetic and, most recently, as an anti-viral drug.
Chloroquine was first produced in 1934, and widely distributed to soldiers who were training or stationed in malaria hot spots during World War II. By 1945, the drug became the standard recommendation for malaria treatment by the World Health Organisation (WHO).
The wide distribution of chloroquine led to the observation that the drug improved rashes and arthritis in soldiers. Not long after, it was prescribed to lupus and arthritis patients globally.
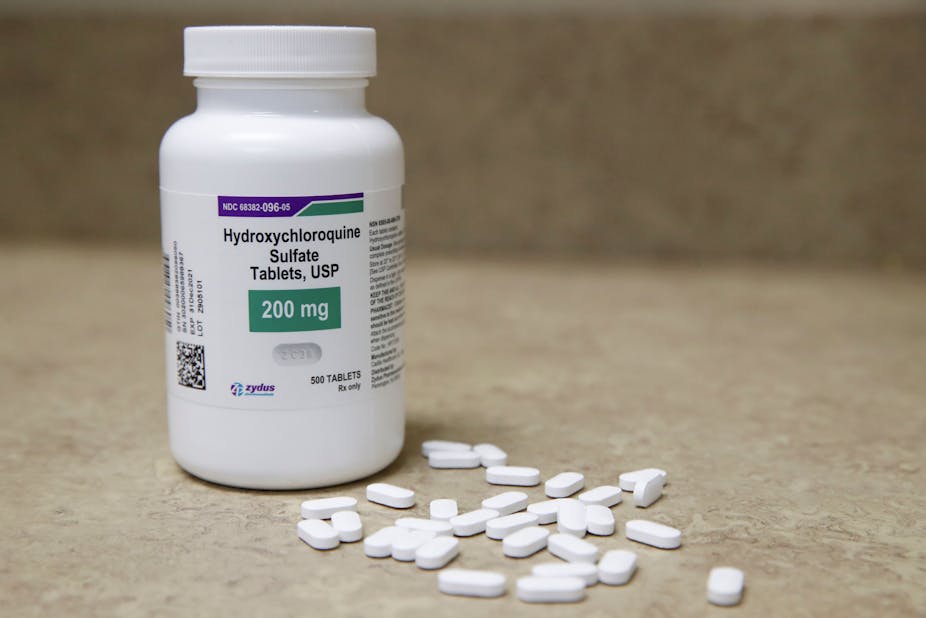
But these patients also suffered from blurry vision, gastrointestinal problems and weakened muscles. To decrease the side-effects of chloroquine, hydroxychloroquine, which is identical to chloroquine with the exception of one chemical group, was produced in 1955 and has been used since.
Observational studies in arthritis and lupus patients who received chloroquine or hydroxychloroquine over a long time period suggested that these patients were less likely to develop type 2 diabetes, and a new role for these drugs as a potential anti-diabetic treatment emerged in 1984.
But reports have also suggested that high doses of chloroquine and hydroxychloroquine can be harmful to the heart. We set out to investigate this and found that there were indeed cardiovascular effects which might outweigh the drug’s advantages. This risk needs to be considered carefully, especially when researchers are looking for quick solutions to urgent health problems.
Anti-diabetic
To understand how hydroxychloroquine works against diabetes, it’s necessary to know something about the human body’s response to food.
Insulin resistance develops when there is a surplus of nutrients present in the diet (for example in obesity) over long time periods. The excess glucose present in the blood stimulates a continuous release of insulin. Cells throughout the body become desensitised to the extra glucose and insulin. They decrease their uptake of both, which influences cell behaviour.
In type 2 diabetes, the body can’t produce any insulin in response to the extra glucose. Hydroxychloroquine stimulates the body to produce more insulin and keep it in the blood for longer by protecting it from being broken down. This gives the cells more time to take up both insulin and glucose.
But this does not come cheap. Hydroxychloroquine can also lower blood pressure, cause an irregular heartbeat and further decrease already low blood sugar levels. All of these are serious side effects.
The advantages and disadvantages of chloroquine and hydroxychloroquine as repurposed drugs have led to a debate in scientific literature about its use and dosages.
Our study investigated the effect of different chloroquine concentrations on the rat heart. We found that a single low dose of chloroquine is enough to significantly decrease heart rate and function. Long-term treatment with low doses of chloroquine worsened heart function in healthy and obese rats and did not improve glucose uptake in the obese animals.
Overall, our study concluded that the side effects of chloroquine on the heart, after as little as a single low dose, outweigh any therapeutic advantages that the drug might have for diabetic patients, especially when there are more effective and less toxic anti-diabetic drugs available.
There have been reports of heart complications in patients with diabetes, arthritis, lupus and malaria treated with chloroquine or hydroxychloroquine. This has been blamed, partly, on the drug’s ability to stop the cellular recycling machinery from working. This also prevents insulin from being degraded and can result in a buildup of toxic byproducts.
Both chloroquine and hydroxychloroquine accumulate in cells over time. It’s believed that this accumulation leads to some of the side effects observed after prolonged use or very high doses. Both drugs are still widely prescribed for arthritis, lupus and malaria, but patients are advised to undergo annual electrocardiograms.
From anti-malarial to anti-viral
Recently, chloroquine and hydroxychloroquine have come to the fore in the search for a treatment for COVID-19. This is because the drugs were shown to prevent viruses from multiplying inside a cell under laboratory conditions.
They were tested against HIV and the human coronavirus that caused the severe acute respiratory syndrome outbreak of 2002-2003. But these studies were mainly done in laboratories and rarely tested in patients.
A recent study (20 patients) in France found that hydroxychloroquine lowered the viral load of SARS-CoV-2, the virus that causes COVID-19. The study did not report any side-effects, but has been widely criticised for design flaws in the methodology. This was followed by a larger study in Brazil where 81 patients were treated with either low or high doses of chloroquine. Within three days of the study, several of the patients developed an irregular heartbeat (arrhythmia). After six days, 11 patients had died. The high dose arm of the study was stopped, citing a 25% increased risk of developing arrhythmia.
The WHO recently suspended the use of hydroxychloroquine in a global drug trial. This followed the publication of a study that showed no benefits from the use of chloroquine or hydroxychloroquine for COVID-19, and suggested that the drugs might actually be harmful. But data from this study and others by the authors could not be independently verified, and have been retracted.
Way forward
At this stage, the scientific community warns that the hype around chloroquine and hydroxychloroquine could derail the search for more effective treatments. There is an urgent need to develop effective treatments against COVID-19. But there are also many pitfalls in small, uncontrolled drug trials, and the accelerated pace at which data is published.
If these drugs are prescribed for COVID-19, it should be done with extreme caution and a detailed risk assessment of the patient. The Food and Drug Administration in the US has warned against the use of chloroquine and hydroxychloroquine outside of a clinical setting or drug trial.
In the hope of finding a cure for COVID-19, it is easy to get lost in the hype and rapid publication of data. For now, chloroquine and hydroxychloroquine should be handled with caution, at least until more information from robust and peer-reviewed studies is available about its effect on the hearts of compromised COVID-19 patients.