It’s been a really interesting month for those of us who follow the chronic pain literature.
The idea that higher brain processes such as attention, emotional functioning and even language can be affected by chronic pain processes has been around for a while. The evidence has been building for a few years that conditions which give rise to persistent pain affect the whole brain and spinal cord, but there have been 4 studies come across my desk this month which elegantly demonstrate unexpected facets of this idea.
The first comes from a group of German researchers who hypothesized that Complex Regional Pain Syndrome (CRPS) may cause a shift in the perceived midline as judged both with visual feedback, and in the dark. The perceived midline is an important measure of spatial awareness as it compares how closely a subject’s idea of where ‘straight ahead’ is with external reality. Conditions such as strokes which damage the parietal and temporal lobes tend to cause dramatic changes in the perceived midline, usually moving it to the left for reasons which needn’t detain us at the moment. The study is in pre-press and will soon be published in PAIN . In graphical form, here is what they found…
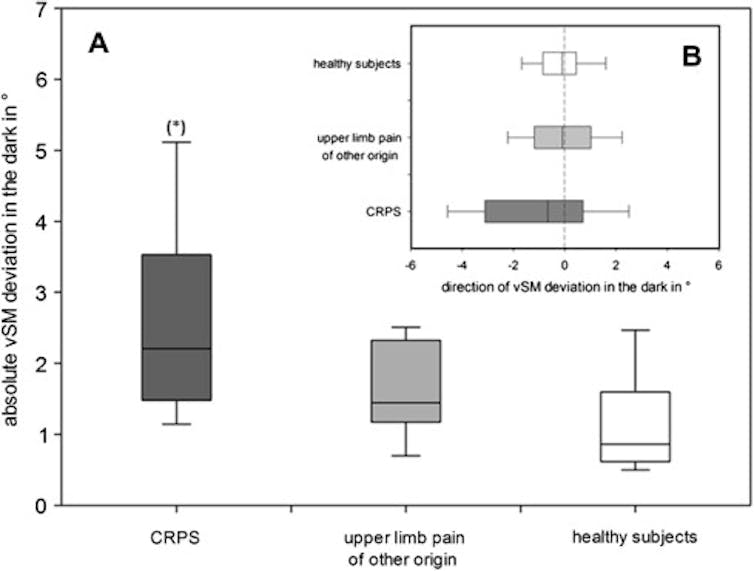
The practical consequence of this study is not obvious. It is profoundly important for understanding the rehabilitation of patients with such pain, as the implication of a shifted midline perception is that the brain is no longer paying attention to that sensory field. In extreme cases, this is called hemispatial neglect and is highly disabling. It is as if the high-level sensory and motor areas have written off any input from that half of the body and the space around it. This dovetails nicely with the clinical observation that in CRPS, constant sensory stimulation and movement of the painful area results in a better outcome. It also jibes nicely with the classic observation that many CRPS sufferers preferentially use their ‘good’ hand to do tasks, even if they have to cross to the other side of their body where the ‘CRPS’ hand could easily reach it.
A second nice study looked at visual attention. Psychological theory holds that perceptual processes give priority to objects in the environment which are assessed as potentially threatening. The evolutionary benefits of such a bias are obvious. If you are a dedicated arachnophobe like my middle son, you are always that first to spot a spider that others seem blind to. If you are thinking seriously about a buying a particular model of car, you seem to start coming across them everywhere. This group of Chinese neuropsychologists extended this reasoning to predict that subjects with a very high fear of pain should react more quickly to visual pain cues. What was particularly novel about their experiment was that it used flashcards with pain-related words on them, ie something of no visual threat value but requiring cognitive processing before the threat value was obvious. They used eye-tracking equipment to show that even without conscious effort on the part of the pain-fearing subjects, their eyes flickered more often towards the pain-related words or ‘health catastrophe’ words than did those with a low fear of pain.
Note that these were healthy adult volunteers, rather than chronic pain patients. This experimental finding is in line with the broader sweep of data that strongly support the idea that tackling fear of pain is a significant step towards normalising brain function in those who have chronic pain. Reducing attentional bias towards bodily pain or threats of pain has long been a major strategy for successful self-managers of chronic pain, but we are now really getting to grips with why that might be so.
The third study of interest involves what is probably the best-named test in the literature…the rodent gambling task. The researchers, this time from Portugal, were investigating another part of the brain thought to be impaired by chronic pain - the orbitofrontal cortex. The OFC is often injured in vehicle accidents, as it sits at the front of the skull right where the brain crashes against the ‘dashboard’ of the eye sockets in a front-on impact. Impaired output of the OFC tends to result in impulsive, emotionally-driven decision making without much reasoning or the ability to prioritize. It may also be significant in social cognition. The Portugese study showed that rats who had electrodes recording their OFC activity would make calculations of reward size, and tended to favour risk-averse, optimal gambling strategies when not in pain. In the presence of an inflammatory arthritis, there was a notable change in the activation of the OFC neurons, and the risk calculations went out the window in favour of a high-risk, high-reward game.

This pattern of performance is seen in humans with schizophrenia, gambling addiction and acquired brain injury of the OFC. The significance of this finding in humans with chronic pain is not known at this point but it is tempting to speculate that the propensity of pain patients to undertake desperate, extreme and usually futile efforts to cure their pain looks more understandable in the light of it.
The final paper up for discussion is this one in which the researchers suspected that people with a persistently painful body part would have no trouble recognising body parts visually, but that they would struggle to extract much abstract information about what they were seeing. Sounds weird? It makes sense if you consider that these people’s brains are likely to be paying less attention to their own painful body part. Our ability to observe and judge the movements of others seems to involve our brain comparing the visual input with how we would make the same movement. Think of the famous clip of the gymnast crashing into the vaulting horse, and your own brain will be running through the same movements…ouch! The reason we flinch is that we have pictured the same thing happening to ourselves. 2 groups of chronic pain patients were recruited, one group with long-term shoulder pain, the other with back pain. Participants were shown some abstract figures representing lifting motions and asked to judge the weight being lifted with various movements of the figures. The team found that, exactly as predicted, back pain patients had lots more trouble judging the weight being lifted by a figure that was using its back to lift, whereas shoulder pain sufferers were worse on the same task where a shoulder was involved, but not a back. For movements that the participants could easily perform themselves, their weight judgements were accurate.
So there you go. Having long-term pain can produce a very different lived experience to not having it, because the pain process can impact upon a number of systems which alter the way external and internal events are filtered and attended to. Maybe the pain experience is so hard to understand because those who have it are walking around with ‘pain goggles’ on that cause them to perceive reality quite differently without being aware of it. It’s an intriguing idea, and one which is proving a fertile field for new science to breed the next generation of treatments.
