In the time that it will take you to read this article, millions of your body’s cells will have died via a self-destruct mechanism known as programmed cell death. This process is part of your body’s normal healthy function and is used to eliminate cells that are no longer needed or which have been damaged in such a way that their continued existence might be a threat.
During our development from single fertilised cells to embryos and beyond, programmed cell death plays an essential role in sculpting anatomical structures.

It helps to form all parts of our bodies from our fingers and toes (dying cells take away the webbing between digits as we develop) to the complex network of connections between the neurons in our brains. For the developing embryo, the death of some cells is just as important as the survival of others.
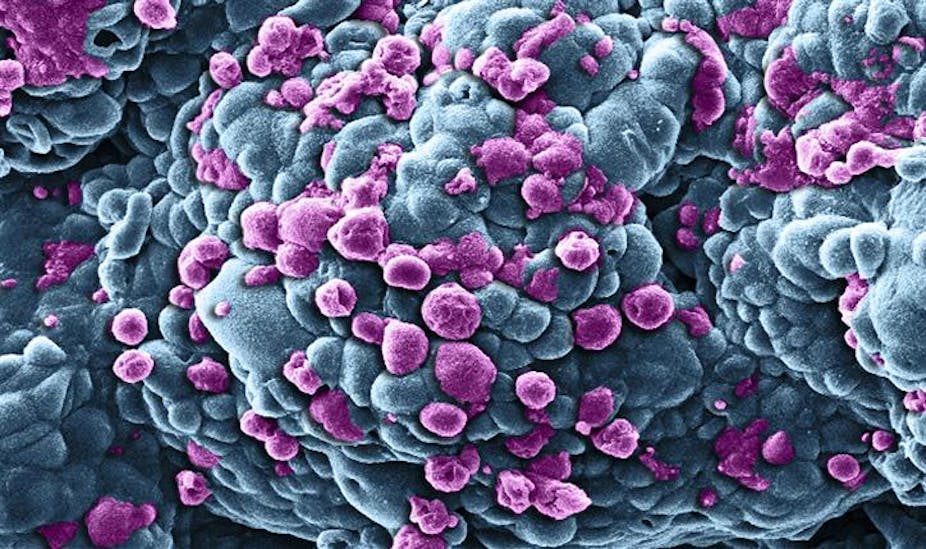
When we’re fully grown, programmed cell death plays an important role in the continuous renewal of tissue such as bone marrow and the lining of the gut. It also acts as a surveillance mechanism – weeding out cells that have been compromised by viral infection or genetic mutation.
Apoptosis, one of the main mechanisms of programmed cell death, gets its name from the Greek word used to describe the shedding of leaves or petals. It was first identified in the mid-19th century but our modern understanding of it dates from 1972 and the pioneering work of John Kerr, Andrew Wyllie and Alastair Currie, then working at the University of Aberdeen.
Neat disposal system
They showed that during this process the contents of a dead cell are neatly packaged up to be absorbed for recycling by specialist white blood cells. This very effective waste disposal system is important because any leaking-out of the cell’s contents could cause harm to the surrounding tissue by provoking inflammation.
We now know that the process of apoptosis is a complex chain of events which involves many different enzymes and proteins. It begins with a signal either that there is something wrong with the cell or that it has become redundant. Sometimes the signal to die is produced by the immune system, but it can arise from within the doomed cell itself.
The message that the cell must die then cascades down to activate enzymes, called caspases, that have been lying dormant within it. These “executioners” then start the process of dismantling the cell according to a genetically encoded programme, and the drama unfolds according to a pre-determined sequence.

However, just as it is important that unwanted or potentially harmful cells are disposed of, it is also essential that healthy cells are not eliminated unnecessarily. Cells therefore also produce survival signals that are able to disrupt the message to commit suicide, and it is the fine-tuned balance between signals for death and survival that ultimately determine a cell’s fate.
Disrupted equilibrium
In cancer, crucially, the delicate equilibrium between cell division and cell death becomes disrupted in favour of too much division and too little death. Disruption of apoptosis is common to all cancers as the uncontrolled proliferation of cells that is characteristic of the disease – for example causing tumours – would ordinarily be a trigger for initiating the apoptosis self-destruct programme.
Normally functioning apoptosis would therefore lead to the death of cancerous cells before they could do any harm. But instead cancer cells suppress apoptosis by either disrupting the signals that tell the cell to destroy itself or by increasing the signals that tell it to survive.
The suppression of apoptosis by cancer cells can make treatment difficult as by definition such cells are more difficult to kill. However, cancers depend on inactive apoptotic pathways for their survival and this is a vulnerability that can be exploited in the treatment of cancer. Reactivate these pathways and the cancer cells might die.

Researchers have already developed cancer drugs that can do just this, either by suppressing survival signals or by restoring the function of death-inducing ones, with promising results.
This work is still in its early days and one major challenge to overcome is the sheer range of different ways that cancer cells find to disrupt apoptosis – use a drug to cut off one of these and the cancer cells may, hydra-like, survive by starting to use another.
Nevertheless, we have come a long way over the past four decades and as we refine our understanding of the complex circuitry of the apoptotic system, the more effective cancer treatments will be developed.