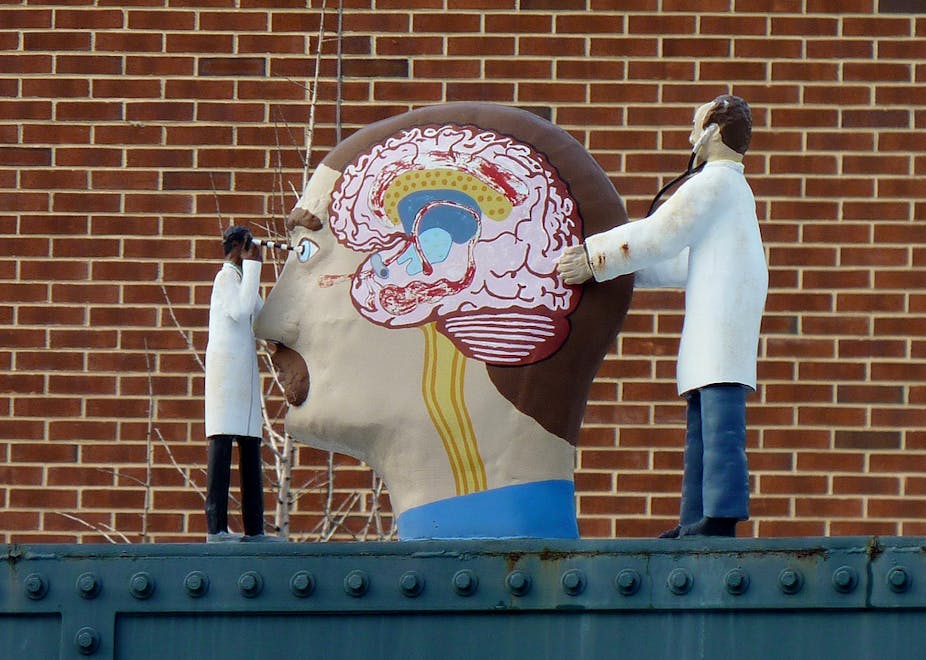
Welcome to part five of _On the brain, a Conversation series by people whose job it is to know as much as there is to know about the body’s most complex organ. Here, Lachlan Thompson, head of the Neurogenesis and Neural Transplantation laboratory at the Florey Neuroscience Institute, explores the brain’s ability to repair itself, with or without medical assistance._
Our brains are finely tuned to perform a remarkable variety of complex tasks. Unfortunately, repairing themselves after injury isn’t one of them.
This means the loss of neuronal circuitry that occurs following damage is permanent, as are the functional consequences for the patient.
So can we rebuild the damaged brain? Clinical trials in patients with Parkinson’s disease (PD) suggest we can.
In PD there’s a progressive and permanent loss of a group of dopamine-producing neurons that form an essential pathway in the brain circuitry controlling movement.
In the late 1970s, researchers in Sweden found if new dopamine neurons are transplanted into the brain they can survive and restore normal control of movement by essentially replacing the damaged circuitry. Since then, more than 300 PD patients have received dopamine-neuron transplants.
While the results have been astonishingly good for some patients, this therapeutic approach is not without its problems.
The procedure relies on the use of human foetal tissue (acquired from elective abortions) and requires anywhere between two and four foetal donors per patient. Hardly a sustainable or, depending on who you ask, ethical resource.
Also, the overall results have been highly variable and unpredictable between patients. This very likely is also related to the use of foetal tissue, which is virtually impossible to standardise in terms of the number and kinds of cells that are grafted into each patient.
Where to now, then?
We know that in principle the therapeutic strategy outlined above has great potential but there’s clearly a need for a better cell source. Enter stem cells.
The hype and expectation surrounding stem cells over the last decade has been impossible to ignore. Most of the excitement in this field surrounds the most powerful pluripotent stem cells that have the ability to generate any cell type in the body, including neurons for brain and spinal cord repair.

The most well-studied pluripotent stem cell is the embryonic stem (ES) cell. These are cells that exist transiently during embryonic development – after a fertilised egg has grown to reach a cell mass of 100-200 cells. They are essentially the “building blocks” for the whole organism.
Most of the ES cells used in research are “extra” embryos created through in vitro fertilization (IVF) procedures. These cells can be grown in large numbers in the laboratory and there are now routine procedures for generating a wide variety of neurons relevant to specific neurological conditions, including dopamine neurons for PD.
While the potential of ES cells for brain and spinal cord repair is undeniable, this is offset somewhat by ethical concerns about their use in medical research. Is it OK to use cells with the potential to generate life as a kind of “spare parts” factory for patients with potentially life-threatening brain or spinal cord injuries? Not everyone thinks so.
Recent groundbreaking work from Japan offers a possible solution. In 2006, a team lead by Professor Yamanaka at Kyoto University discovered a method that converts normal adult cells (e.g. skin cells) into pluripotent stem cells called “induced pluripotent stem (iPS) cells”, which essentially have all the properties of ES cells. This is discussed in the video below.
The method discovered by Yamanaka may lead to therapies in which patients can use their own cells as a “repair-kit” to generate new ones for brain repair. It has also opened an interesting new area in stem cell science where iPS cells can be established from patients to model certain diseases in the laboratory dish.
Stem cells and you
Australian scientists are making progress in this area. Recently, researchers at the University of Melbourne – Dr. Mirella Dottori and Dr. Alice Peabay – have established iPS cell lines from patients with Freidrich’s Ataxia, providing a valuable new research tool in the fight against this debilitating disease, which affects the heart and central nervous system.
Similarly, scientists in Boston have created dopamine neurons from iPS cells and found they can survive and improve motor function after transplantation in an animal model of Parkinson’s disease.
When will we see stem cell based procedures available for patients? While the stage is now set for the development of stem cell treatments for brain repair, a considerable amount of work still needs to be completed before we see these as safe and effective mainstream therapies.
In the meantime, a worrying consequence of the hype surrounding stem cell research has been the rise of so-called “stem cell tourism”. Patients who have exhausted conventional treatment options are increasingly being attracted by clinics in countries such as China, India, Malaysia and the Philippines to receive stem cell treatments.

The procedures are typically expensive and performed in an unregulated environment with little or no scientific basis to suggest a positive outcome. Anecdotally, there have also been a number of examples of patients returning home with acute, and potentially life-threating, complications arising from the treatment.
This phenomenon adds further urgency to the need to develop regulated therapies built on solid scientific evidence.
Much of the pre-clinical research required in this area will focus on understanding exactly how stem cell preparations integrate into damaged circuitry after transplantation and how to standardise the procedures in order to deliver predictable therapeutic outcomes.
There is also an important safety aspect to consider. The powerful nature of stem cells means there’s a risk that, if the wrong cell types are transplanted, they may continue to grow and give rise to tumours.
Such hurdles need to be overcome before we see what has been a very promising period for stem cell biology in the laboratory translated into real outcomes for patients.
This is the fifth part of our series On the brain. To read the other instalments, follow the links below:
Part One: Picking your brains: what’s going on inside your head?
Part Two: Your brain knows the moves (you just get in the way)
Part Three: Brain’s addiction: what makes heavy drug users different?