We first identified Variant Creutzfeldt-Jakob disease at the University of Edinburgh in 1996. This neurological disorder, which is caused by abnormal proteins called prions that infect the brain, was initially found in 12 British patients. Since then 177 cases have occurred in the UK, with 52 cases in 11 other countries.
vCJD belongs to a rare but fatal group of prion diseases and first appeared in people who had eaten meat products contaminated with bovine spongiform encephalopathy (BSE) – or “mad cow disease” – during the 1980s and 1990s. While vCJD is a recent member of this group of diseases, the most common is sporadic sCJD, which was first described in the 1920s and affects one or two people in every million of the population.
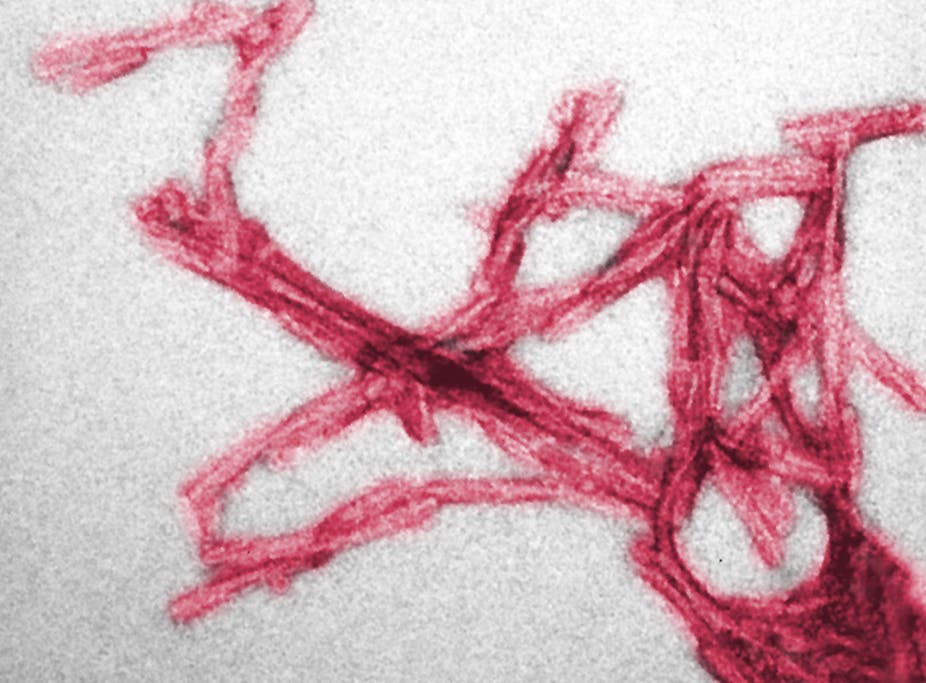
Unlike more common neurological conditions such as Alzheimer’s, prion diseases are transmissible. Prions are very different from conventional bacteria and viruses and appear to spread by converting normal proteins on the surface of cells. BSE prions cross the wall of the gut after infected meat is eaten, before replicating in lymphoid tissues such as the spleen, tonsils, and appendix and they eventually spread to the blood and finally to their target – the brain.
We wanted to know if prion proteins were detectable in lymphoid tissues before the onset of clinical signs and symptoms of vCJD, and they have been found in appendix tissues surgically removed (because of appendicitis).
Once these prions reach the brain, they accumulate and cause the degeneration and death of nerve cells. They are also resistant to normal methods of decontamination – such as sterilisation – and sCJD has occasionally been spread by accident through neuro-surgical instruments that have been on the brain of sCJD patients.
Incubating the disease
In order to find out how many people in the UK might be incubating vCJD, but showing no symptoms, a series of studies were performed on appendix and tonsil samples that were removed from otherwise healthy individuals who were likely have to have been exposed to BSE during the epidemic. The latest and largest of these studies, which was published last year in the BMJ, found 16 out of 32,441 appendixes to be positive, suggesting that one in 2,000 of the UK population might be incubating vCJD.
While the neurological illness in all forms of CJD is usually measured in months, the incubation period is lengthy and can be estimated in years, if not decades. And as vCJD has been transmitted by blood transfusion from UK donors who were incubating vCJD (with no symptoms of the disease at the time of donation) to four different recipients, this raises concerns that vCJD might continue to be transmitted by blood transfusion in the UK, making it difficult to control.
Finding a simple way to test
Given the possible risks of transmission of vCJD by blood transfusion and surgical instruments, there is a pressing need to develop a series of screening tests. But at present there is no test available to find out who might be incubating vCJD or sCJD – a diagnosis is only made after the onset of the neurological problems such as rapidly progressive dementia, unsteadiness, loss of vision and immobility.
But research is making progress. This month we published the results of a new test to detect vCJD prions in the urine of patients, which we published in the New England Journal of Medicine. This test was developed by Claudio Soto in the US (with collaborators in the UK National CJD Research & Surveillance Unit, in France and Italy) using a pioneering technique known as protein misfolding cyclic amplification (PMCA). This technique can detect very low levels of prions in tissues and body fluids that escape detection by conventional methods.
The test did not give positive results in urine from patients with sCJD, other neurological disorders, or in normal individuals. But it is the first time that we’ve been able to detect prions in the urine of patients with vCJD. It opens the door to the next development, a screening test to detect infection in individuals who do not show any symptoms, which is of particular concern in the UK.
Other groups across the world are working on other tests for vCJD, including blood tests, so hopefully in the future a number of screening and confirmatory tests will become available.
Not everyone gets vCJD
Exposure to BSE is likely to have been widespread in the UK, where up to 3m infected cattle may have entered the human food chain. It has therefore been questioned why the total number of vCJD cases in UK is not higher and is now in decline. Possible explanations include the protective effect of a “species barrier” between cows and humans, age-related susceptibility, and genetic factors: all patients with definite vCJD have a similar genetic feature in their prion protein gene.
The recent report published by the House of Commons science and technology committee said:
While cases of vCJD are now rare, recent studies indicate that tens of thousands of people in the UK might be ‘silent’ carriers of the prions responsible for the disease and could perhaps transmit those prions to others. The most likely form of onward transmission is through blood transfusion. Cases of transfusion-transmitted vCJD are known to have occurred in the past, and, while it remains to be seen whether or not widespread transmission via the blood supply is probable, evidence suggests that it is possible.
In the absence of a validated test capable of detecting the presence of prions in blood, we simply cannot know how significant a threat to public health vCJD might be.
We hope that research and progress being made in this area will change this.