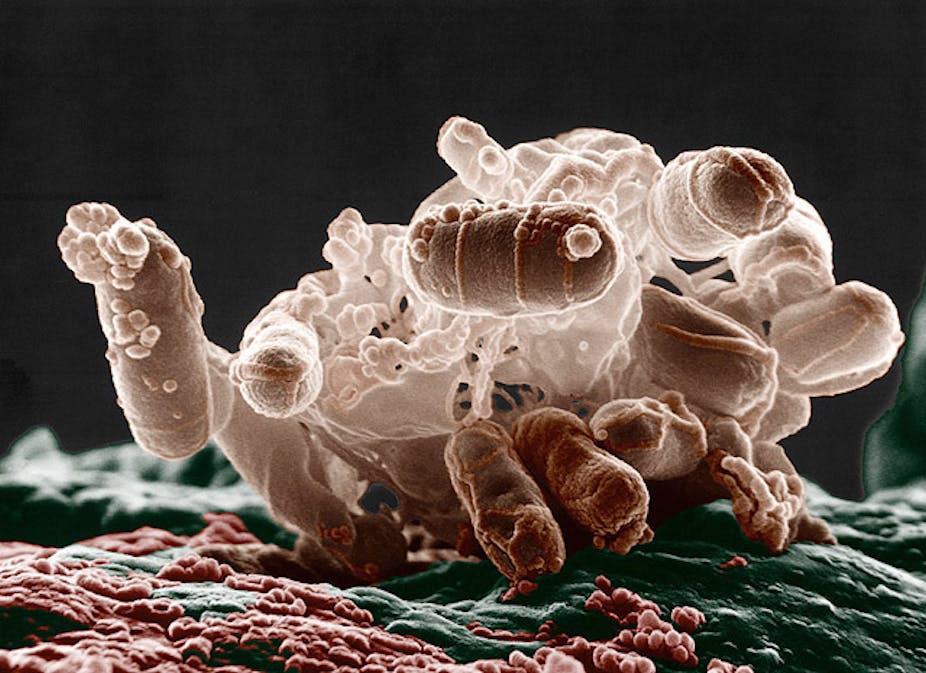
Bacteria are single-celled microorganisms abundant in nature that can’t be seen with the naked eye. In fact, there are approximately five multiplied by 10³¹ bacteria on the earth, constituting 90% of its biomass.
These microorganisms are found everywhere in our environment and are vitally important to maintaining a balanced ecosystem. They cycle carbon, nitrogen, sulphur, hydrogen and oxygen, regulate and affect the growth of plants and animals, and are at the base of most food chains.
Microorganisms also play a pivotal role in human health, as most areas of our body that come in contact with the outside environment, such as the skin and gastrointestinal tract, harbour resident (colonising) bacteria. In fact, there are about ten times as many bacterial cells inside and on you than there are human cells.
These colonising bacteria don’t cause disease under normal conditions. They actually protect us by preventing the growth of harmful bacteria. But sometimes colonising bacteria can get past the body’s defence mechanisms, invade underlying tissue and cause an infection. This occurs most often when people are unwell and their immunity (or ability to fight infection) is diminished.
In addition to environmental sources, bacteria are also able to spread from person to person through close contact. This is generally not problematic as we are able to remove these transient bacteria with natural defence mechanisms and regular washing. But when we’re ill, the ability to clear transient bacteria from our hands or skin is reduced. These bacteria can then invade and cause infections.
Not surprisingly, this phenomenon is most commonly seen in hospitals where many ill people are close to each other. When bacteria are spread to multiple patients over a short period of time, there’s an outbreak of disease.
Antibiotics are generally used to fight these infections, but bacteria are able to fight back and evolve resistance, making the medicines ineffective. They do this by getting DNA that confers resistance from other bacteria through cell-to-cell transfer (or conjugation), bacterial viruses or natural uptake of DNA released from other cells.
A bacterium’s own DNA can also randomly change due to errors that occur when cells make copies of themselves. Sometimes these changes can also confer resistance by mechanisms such as changing the site the antibiotic targets.
Bacteria are masters of adaptation in this respect and, in some cases, have become resistant to all known antibiotics. Worryingly, the development of new antibiotics is slow and without more prudent use of existing ones, it’s likely that the number of people with untreatable infections will steadily increase.

The complete DNA makeup of an organism is referred to as its genome, and its constituent part, the DNA-helix, is made up of subunits called nucleotides (or bases). The human genome is composed of approximately three billion bases. In contrast, bacterial genomes can range in size from 0.1 to 13 million bases.
All functions in bacteria (as in humans) are determined by the genome, and being able to determine a bacterium’s DNA sequence enables us to gain many important insights. This has not been possible on a large scale until quite recently. The development of whole-genome-sequencing technologies means we are now able to sequence several bacterial genomes in one or two days.
This is useful information because it allows us to understand changes in bacteria that enable them to invade the body. Bacterial genome information shows us DNA alterations or mutations that allow bacteria to switch from being a coloniser to an invader.
It can also provide us with an understanding of which strain or type of bacteria is dominant within a specific hospital setting, such as an intensive care unit.
Together, these factors help researchers and medical professionals develop ways of preventing life-threatening infections. Understanding the genome dynamics of the bacterium Neiserria meningitidis (meningococcus), for instance, facilitated development of the meningitis vaccine. This vaccine now forms part of the general immunisation schedule and saves numerous lives each year.
Bacterial genome sequencing also allows us to study how bacteria develop antibiotic resistance. This provides opportunities such as developing more effective drugs. In other words, we can alter antibiotics to overcome identified mechanisms of resistance.
And it allows us to understand how bacteria cause outbreaks and track the spread from person to person, ultimately preventing patients from developing associated infections.
Being able to readily determine the DNA sequence of bacteria can facilitate disease prevention in many different ways. And that dramatically improves the potential for positive patient outcomes.
The field of bacterial genomics (and genome sequencing in general) is inspired and driven by landmark achievements, such as completion of the first Human Genome Project. It is now conceivable that, in the not too distant future, bacterial genome sequencing will be routinely used by infectious disease specialists to guide patient care.