Our cells are up against a daily onslaught of damage to the DNA that encodes our genes. It takes constant effort to keep up with the DNA disrepair – and if our cells didn’t bother to try to fix it, we might not survive. The DNA damage repair pathways are an essential safeguard for the human genome.
The 2015 Nobel Laureates in chemistry received the prize for their pioneering work figuring out the molecular machinery that cells use to repair that DNA damage. In their basic research, Tomas Lindahl, Paul Modrich and Aziz Sancar each narrowed in on one piece of the DNA repair puzzle.
They’ve laid the framework for the research that many basic and translational scientists are expanding upon to try to crack cancer. Ironically, we’re finding ways to turn that DNA repair system against cancerous cells that have often arisen from DNA damage in the first place.

DNA under siege
DNA is composed of four simple letters, or nucleotides, A, T, C and G. When combined, these nucleotides form the genetic code. There are approximately 30,000 genes in the human genome.
Each time a cell grows and divides, every single gene needs to be faithfully copied to the next generation of cells. This process of DNA replication is constantly threatened by both internal and external sources of DNA damage. There are environmental sources such as radon from the earth or UV light from the sun. Or it can be just a mistake, happening within the cell as a consequence of normal growth and division. Some studies have estimated that a single cell can experience several thousand DNA damage events in a single day.
The question then becomes: how does the cell repair all of this damage? Or perhaps more worrisome, what happens if the cell doesn’t repair the damage?
A full toolbox to deal with the damage
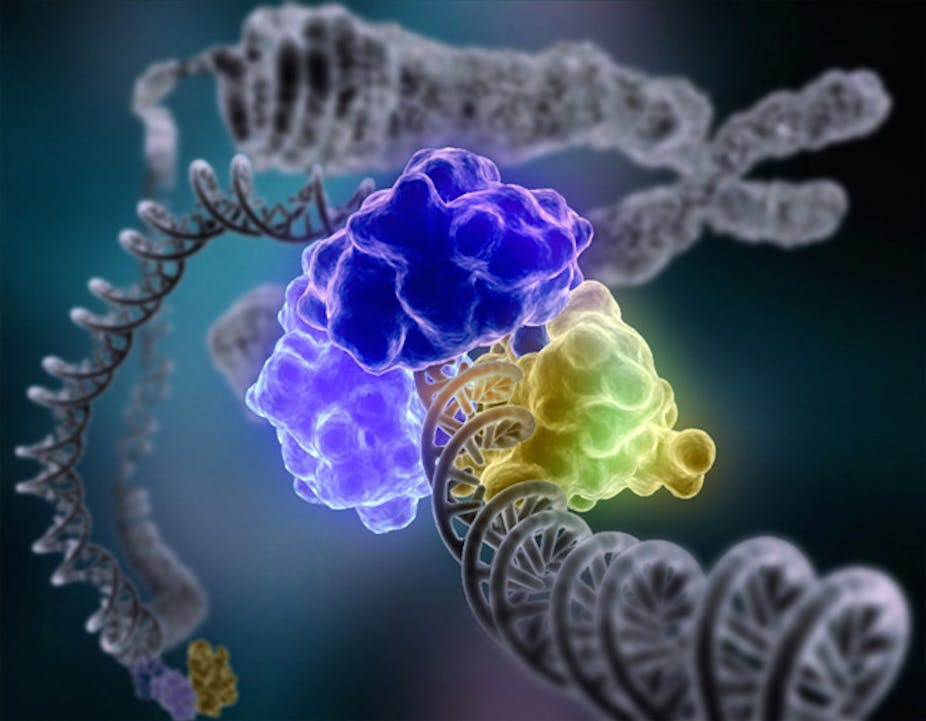
To counter the daily onslaught of DNA damage, mammalian cells have evolved a number of intricate mechanisms to not only recognize DNA damage, but repair it and restore the original genetic sequence.
Consider a typo that changes the letter N to the letter M, causing “grin” to become “grim.” That single typo has now changed the entire meaning of the word. It works just the same in the “words” of the genetic code when an incorrect nucleotide takes the place of the right one. The DNA damage repair enzymes function like an eraser reverting the mutant M back to the original N.

Following DNA damage, the cell must first recognize the damage and then alert the system that there’s a problem. The recognition machinery then activates various factors to halt cell growth until the damage has been repaired. And if things are too far gone, additional factors are poised and ready to induce cell death.
That’s the most basic way to think about the DNA damage response pathway, as a simple chain of events. Of course it’s a lot more complicated, a complex network of checks and balances to ensure that the DNA damage is not only recognized but clearly identified to ensure that the correct factors are recruited to repair the lesion.
Much like a homeowner wouldn’t want an electrician to fix the leaky roof, a DNA “typo” shouldn’t be fixed by a mechanism used to heal double-strand DNA breaks, for instance. Therefore, sensing which specific genetic lesion is the problem is one of the earliest and most critical steps in the DNA damage response pathway.
It’s hard to say exactly how many DNA damage response “sensors” there are or exactly who they are, but that’s something the field is actively investigating. Likewise, while the number of DNA damage repair pathways we know about hasn’t necessarily increased since the groundbreaking Nobel work was done, the complexity of our understanding has.
What if the repair process itself is broken?
In a limited capacity, mutations actually aid evolution. There have to be changes for natural selection to act on, so these DNA mutations are a significant factor in Darwin’s theory of evolution. However, what is a blessing may also be a curse.
Mutations in essential genes can lead to death even before we enter the world. However, mutations in nonessential genes may not be evident until later in life. When these mutations persist – or even worse, accumulate – it can lead to genomic instability. And that’s a hallmark of cancer cells.
You can imagine, then, that a single mutation in a component of the DNA damage response pathway could lead to the accumulation of DNA damage, genomic instability and ultimately the progression toward cancer. And it’s true, we frequently find mutations in the DNA damage response pathway in cancer. Deciphering exactly how these pathways work is essential to our understanding not only of cancer, but also of how we might exploit these pathways to actually treat the disease.
Harnessing the repair systems to our own ends
These damage repair pathways are essential to prevent the accumulation of genetic lesions and ultimately inhibit the progression toward cancer. Is there a way we can exploit the system, push it over the edge and cause an unwanted cell not just to gain mutations but to die?
To that end, researchers are hard at work trying to further define the nitty gritty details that regulate the DNA damage response. Others are trying to identify factors that we could target therapeutically.
It may seem counterintuitive to target the DNA damage response pathway once it’s already been inactivated by a mutation. But the approach has its advantages.
Generally, when a genetic mutation inactivates one branch of repair, the cell will try to compensate by using another type of repair just to keep the cell alive. Would you rather call the electrician and hope he can fix the leaky roof or risk having the entire roof collapse in on you?
The cell opts for a back-up mechanism to try to resolve the damage. In general, this results in inadequate repair and the acquisition of additional mutations, fueling the genomic instability and cancer progression.
We want to eliminate the back-up mechanism – send the electrician out of town. Research has demonstrated that when one type of repair mechanism is inactivated by a genetic mutation and you therapeutically inactivate the back-up mechanism, the cancerous cell dies. Likewise, if we combine drugs that induce a particular type of damage and then inactivate that specific repair pathway, cells die. Clinical scientists have demonstrated that this can lead to tumor regression in patients sparking a surge of research in this area.

Targeting telomeres
My lab is interested in understanding how the DNA damage response is regulated specifically at telomeric DNA.
The telomere is a repetitive DNA sequence that caps the ends of each human chromosome. Telomeres function as a barrier, protecting the human genome from degradation and/or the fusion of whole chromosomes.
Each time a cell divides, a portion of this barrier is lost; over time the shortened telomere compromises the genome’s stability. To avoid damage to the genome, critically short telomeres send a signal to the cell to either stop growing or induce cell death.
Cancer cells, however, have evolved mechanisms to overcome progressive telomere shortening and bypass this growth arrest. In other words, they outmaneuver the normal routine, dividing and growing while avoiding the usual step of telomere shortening that eventually leads to death for normal cells. One way they counter telomere shortening and promote telomere elongation is by activating the Alternative Lengthening of Telomeres pathway (ALT).
The ALT mechanism is active in 10%-15% of all human cancers. This incidence skyrockets to approximately 60% in some of the most aggressive forms of human cancer, including osteosarcoma and glioblastoma. These cancers are often resistant to common therapeutic strategies and there are no therapies that specifically target the ALT pathway.

In my lab, we’re focusing on one of the molecules that senses DNA damage in the first place, the ATR kinase. We’ve found that preventing it from doing its job leads to both a decrease in recombination at telomeres and an increase in telomere loss at the chromosome ends, suggesting a defect in ALT activity.
Perhaps most significant is that ATR inhibitions led to catastrophic cell division and robust cell death in ALT-positive cancer cells, yet had little effect on non-cancerous cell lines.
These studies may allow us to drive ATR inhibitors into preclinical development with the ultimate goal of improving the therapeutic strategies in the treatment of some of the most aggressive forms of human cancer.
It’s this kind of translational research that builds on the framework laid by the work of our newest Nobel laureates in chemistry. Their basic research is proving to be the foundation for new ways to target – and hopefully treat – cancer.