Patients recovering from heart attacks are almost 30% more likely to take part in rehab at home using a new smartphone app compared to those who had to travel to an outpatient clinic or centre.
What’s more, those who used the online delivery model – known as the Care Assessment Platform – were 40% more likely to adhere to the rules of the program and almost 70% more likely to see it through to completion.
The clinical trial, conducted by CSIRO and Queensland Health through the Australian E-Health Research Centre, also showed that the online model was just as clinically effective as a traditional rehab program.
Cardiologists were so pleased by the results that the next generation version of the platform is soon to be offered in a number of Queensland hospitals including Ipswich, Metro North and West Moreton Hospital and Health Services.
Why go digital?
Clinical guidelines recommend patients attend and complete a cardiac rehabilitation program following a heart attack. Studies have shown that those who do this have much better long-term health outcomes.
They are less likely to be re-admitted to hospital and will have a better quality of life. Most importantly, they are far less likely to have another cardiac event or die from their condition.
Traditionally, rehab programs take the form of group-based exercise, nutritional counselling, risk factor assessment and educational activities. They are designed to help patients return to an active, satisfying life.
Despite the benefits, uptake is generally poor. Successful recovery relies on patients starting and completing a rehabilitation program, but many find travelling to a health care facility on a weekly basis to be an onerous requirement – particularly for those who work or care for others, or live in regional or remote Australia where these services are not available.
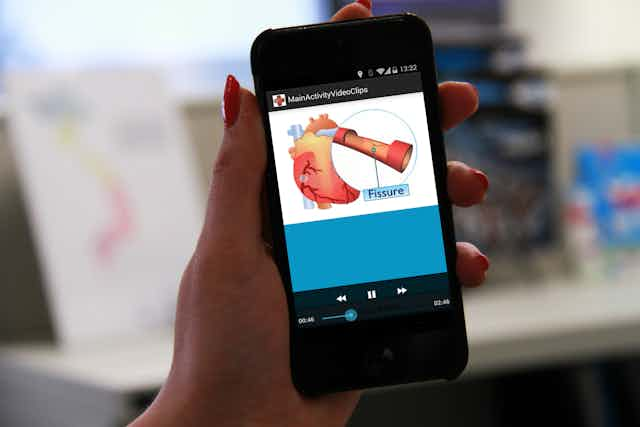
The Care Assessment Platform features health and exercise monitoring tools, weekly mentoring consultations, delivers motivational materials through text messages and contains multimedia that educates patients about disease symptoms and management.
Most importantly, it gives patients a more flexible option. By integrating rehab treatment with a patient’s daily life, they are more likely to complete the program and make their new healthy lifestyle permanent. This overcomes one of the key barriers to patient participation and recovery.
The cost of heart disease
There have been huge advances in our treatment of heart disease in recent years. Researchers from the University of New South Wales have shown that rapid response teams, first introduced in Australia in the 1990s, have halved cardiac arrests and associated deaths in our hospitals. This saves around 12,000 Australian lives each year.
Despite the success of innovations like this, cardiovascular disease still kills one Australian nearly every 12 minutes. And for many of these patients, it is not their first cardiac event.
With more than A$5.5 billion spent every year on acute and chronic management of heart disease, any digital technology that improves recovery rates offers huge potential to reduce the burden and cost to the community.
What does a fully digital health system look like?
Australia’s health system faces significant challenges including rising costs, an ageing population, a rise in chronic diseases and fewer rural health workers. Total government expenditure on health has trebled in the last 25 years.
Clearly, something needs to change.

We must reduce the reliance on our hospitals by helping patients before they are admitted. Digital tools can do this by moving many services into the home through broadband delivery and models of care based on rich digital information.
In another study, CSIRO is running Australia’s largest clinical telehealth trial. In this trial, we’ve equipped a group of elderly patients with broadband-enabled home monitoring systems.
Patients can use machines to measure vital signs such as blood pressure, blood sugar, heart abnormalities, lung capacity, body weight and temperature.
Data is then immediately available to the patient’s doctor or nurse, allowing them to provide appropriate care interventions much earlier. This helps patients stay out of hospital and improve their quality of life.
Ultimately, those patients who are chronically ill will still need to attend hospital on occasion, so technology also has a role to play in improving the effectiveness of our admission systems.
Emergency departments are critically overcrowded and struggle to respond to day-to-day arrivals in a timely manner. Big data analytics can be used to predict how many patients will arrive at emergency, their medical needs and how many will be admitted or discharged. This can then be used to calculate how many beds will be required to meet patient’s needs.
New app-ortunities
The next step for our Care Assessment Platform research team is to adapt our mobile technology for rehabilitation for other chronic conditions such as pulmonary disease and diabetes. We’re also working hard to quantify the cost savings the program can deliver.
Australia has a track record in finding cures and new treatments for diseases. In order to sustain this, we also need to find new ways to deliver quality affordable care.
There is enormous potential for big data, analytics and decision support systems to help achieve this, reducing the burden on our health system and improving the wellbeing of all Australians.