The current outbreak of Ebola in West Africa has emerged rapidly and evolved with alarming ease. An unprecedented number of lives have been lost and WHO predictions are that the virus will infect in excess of 20,000 people before the situation can be brought under control.
This is an extraordinarily challenging time for the nations affected, many of which have fragile, inadequate health infrastructures and have been unable to contain the outbreak.
International efforts are now required to strengthen and implement comprehensive emergency response strategies across the areas affected and most at risk.
Accelerated development
An important part of the measures to be implemented involves fast-tracking access to treatment and vaccine options in order to reduce morbidity and mortality rates and help stop transmission. The gravity of the current epidemic is such that for the first time in history an international consortium has been assembled in order to accelerate the development and deployment of potential Ebola vaccines.
At the Jenner Institute in Oxford we will run the first phase I trial of a vaccine targeted at the Zaire strain of Ebola virus that is causing the current outbreak. The main purpose of this first-in-humans trial in the UK is to establish a detailed safety profile of the vaccine and assess the type of immune responses it induces before it could be considered for widespread use. A further goal is to identify the most suitable dose of the vaccine.
The vaccine is being co-developed with GlaxoSmithKline (GSK) and the National Institutes of Health who are running parallel human phase I trials in the US. Our trial is being funded with a £2.8m grant from the Wellcome Trust, the Medical Research Council and the UK Department for International Development.
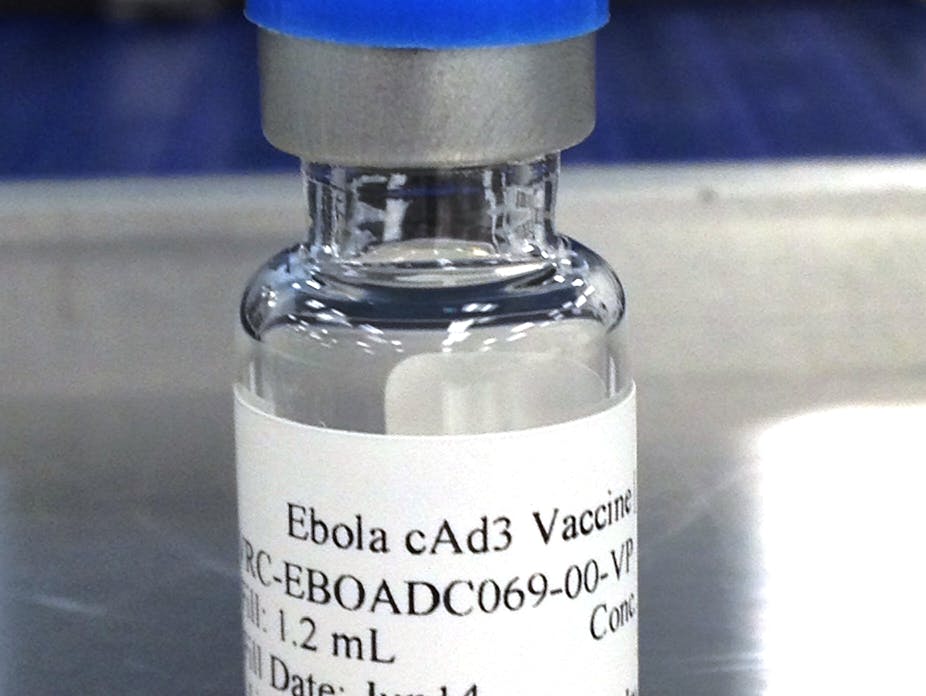
Chimpanzee adenovirus

The candidate vaccine in question uses a chimpanzee adenovirus (a type of respiratory virus) as a means to expose or prime the immune systems of volunteers to a specific protein that exists on the surface of the Ebola virus.
The vaccine contains some genetic material but not the entire Ebola virus genome so it cannot cause an Ebola infection. As with the US trial, the adenovirus also will not replicate but instead prompts the person vaccinated to express an Ebola vaccine that the immune system will later recognise if the person became infected.
Previously it has been tested in animal models and has demonstrated impressive effectiveness at protecting against infection and promoting recovery from animals later exposed to Ebola. Just a single dose was required to induce very high levels of protective efficacy.
Chimpanzee adenoviruses have been used extensively in clinical trials for malaria, hepatitis C and other infections but no vaccine of this type has been licensed as yet. In the 25 clinical trials of chimpanzee adenoviruses that have taken place, the safety profile of this type of vaccine has been good.
At present, ethical and regulatory approvals are being prioritised so that the trials may begin in the UK in September 2014. This will be run in parallel with a cohort in the US and extended to The Gambia and Mali thereafter – subject to agreements on ethical and clinical protocols. At the same time, 10,000 vaccine doses will be stockpiled by GSK in order that, should the vaccine meet safety requirements, it may be deployed without any further delays.
The candidate vaccine will be tested in 60 healthy volunteers over the age of 18, who we will shortly begin recruiting. During the trial volunteers will be administered a single dose of the vaccine into the muscles of the upper arm and blood samples will be taken at specific time points.
In all, volunteers will be expected to attend for a total of nine clinic visits over six months. Clinical trials are an essential part of the vaccine development process and invaluable tools when it comes to understanding and ultimately improving the processes that provide vaccine-mediated protection from disease. In order gain the upper hand over Ebola, we need all the help we can get.