The recent award of the 2023 Nobel prize in physiology or medicine to Katalin Karikó and Drew Weissman highlights the growing importance of RNA technology in the medical world, with many potential applications beyond COVID vaccines.
But until now, one of the major hindrances in making this technology more widely available globally, and in translating research into clinical use, has been the need for proprietary products, often licensed by pharmaceutical companies.
Detailed methodology to deliver RNA vaccines to cells was also not easily available to the research community.
For these reasons we have published a protocol detailing how to make and package RNA with commercially available reagents.
How RNA therapies work
RNA stands for ribonucleic acid. It is a type of genetic material, which can act as a messenger (mRNA), that translates information held in DNA into specific proteins.
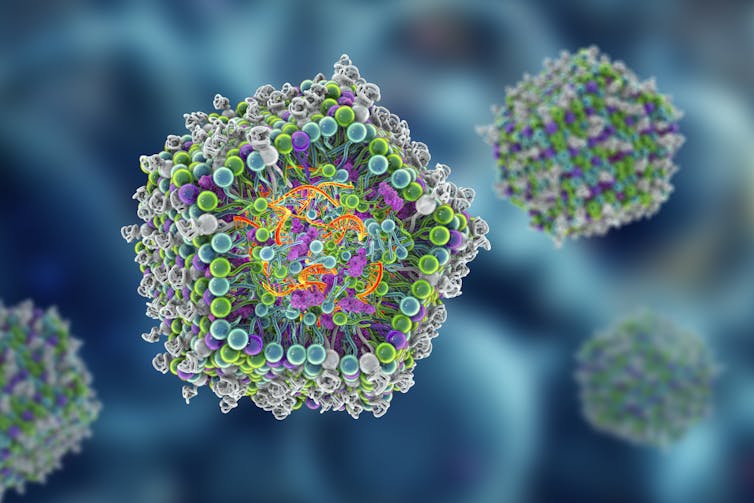
The concept behind RNA therapies is elegant and simple, in theory. There are two distinct components: the RNA payload and the fatty envelope, made of lipid nanoparticles, which safely delivers the payload to cells.
Once inside a cell, the lipid envelope releases the RNA, enabling it to act as a messenger that will be read and translated to make specific therapeutic proteins. In COVID vaccines, the manufactured protein mirrors the spike protein of the SARS-CoV-2 virus, training our immune system to recognise and remember it for a robust future immune defence.
Read more: Messenger RNA: how it works in nature and in making vaccines
It is hard to believe now, but even in the early 2000s RNA therapies were widely considered to be a pipe dream. There were several hurdles in place that, until relatively recently, were considered insurmountable.
Karikó and Weissman’s discovery revolutionised our understanding of how cells detect and react to different RNA structures.
Their discovery allowed therapeutic RNAs to be synthesised so they could avoid destruction by the body before the RNA had a chance to carry out its task. Their seminal paper was published in 2005 – 15 years before the COVID pandemic.
Read more: Beyond COVID vaccines: what else could mRNA technology do for our health?
Delivering the message
Throughout this time, a viable delivery system was being developed as well. RNA is a negatively charged, unstable molecule and cannot maintain its structure in the body without some sort of protective casing.
It was only in the 2010s that lipid nanoparticles were developed and identified as a potential mechanism for delivery.
Two critical advancements are essential. First, the lipid nanoparticles are ionised. This allows the encapsulation of the negatively charged RNA with a positively charged envelope. Then, before injection into the body, this assemblage is converted to a neutral pH, reducing potential toxicity in the body.
Second, a method to achieve consistency in the particle size of the lipid nanoparticles was developed. Size consistency matters because it enhances the vaccine’s uptake by cells in the body.
Time in the spotlight
By the time the COVID pandemic arrived, the essential components to make a viable RNA vaccine had emerged. RNA vaccines were especially appealing as they can be rapidly synthesised in the lab using just the genetic code of the virus.
As a result, the research field progressed rapidly. In addition to pharmaceutical development, several research groups around the world started work on RNA technology, applying it to a plethora of different diseases, including cancer, gene therapy and vaccines for different infectious diseases.
However, intellectual property constraints surrounding the lipid nanoparticle envelope raised production costs and affected investment prospects. This meant that while research and design could move forward, taking the findings into the clinic was not possible without paying the premiums to license certain reagents.
The result has been that labs around the world are developing their own techniques from scratch, leading to a grossly inefficient system.
The democratisation of RNA technology
Our research expedites the method development process by providing a springboard others can launch off. It is a standardised technique researchers can use as a baseline for RNA therapies without the need for proprietary products.
This will mean more people around the world will be able to bring RNA technology into the clinic, broadening its scope, impact and safety.
Current lipid nanoparticle formulations have also been optimised for a generalised immune defence, rather than specific tissue-targeted immune responses. Unhindered research in this area may unlock findings that allow very specific organs or even cells to be targeted.
It will also enable more universities and even schools to teach and research this technology and improve it for applications beyond those that will be commercially profitable.
We have only seen the tip of the iceberg in terms of the therapeutic potential of RNA technology. By democratising this technology, we can more fully explore and harness its myriad possible therapies.
The protocol was developed in collaboration with Te Kāuru – Ferrier Research Institute at Te Herenga Waka Victoria University of Wellington.

