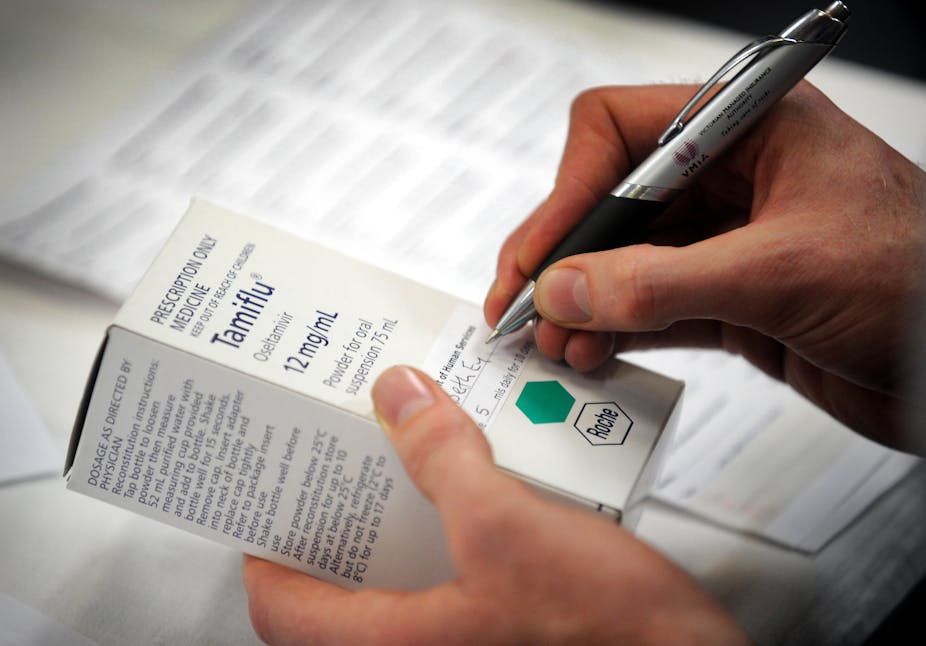
A team of public health experts has called for the release of all clinical drug trial results for independent analysis following a “frustrating” three-year battle for access to data on controversial flu drug Tamiflu.
The team, which includes Bond University Professor of Public Health Chris Del Mar, says that in the case of Tamiflu - stockpiled by many countries at enormous cost to taxpayers - drug companies, drug regulators, and public health bodies such as the World Health Organisation have all made discrepant claims about its clinical effects.
Despite a recent review that raised questions about the efficacy of Tamiflu, the drug remains on the World Health Organisation’s List of Essential Medicines.
“The manufacturer, Roche, has made some $4.6 billion worldwide from sales of Tamiflu, most of which is down to governments buying it and stockpiling it in warehouses,” Professor Del Mar said. “Australia bought almost $200 million worth of Tamiflu. That’s an enormous opportunity cost if the stuff doesn’t work. So it’s really important that it undergoes the most rigorous analysis.
"We can’t do that analysis if the manufacturer doesn’t make it available for us to look at.”
On several occasions in recent years, health bodies in Japan have raised concerns about the side-effects of Tamiflu after children who were taking the drug apparently committed suicide or harmed themselves.
“We are worried about the side-effects of [Tamiflu], which have been inconsistently reported,” Professor Del Mar said. “It’s another reason why we need the data. This stuff is being used all over the place in huge quantities. The drug company is applying its own censorship. ‘Trust us, we made it and we’re making a big profit from it.’”
With co-authors Peter Doshi from Johns Hopkins University School of Medicine in the US, and Tom Jefferson from the Cochrane Collaboration in Italy, Professor Del Mar has written a paper in this week’s PLoS Medicine arguing that there are strong ethical reasons for ensuring all clinical study reports are publicly accessible.
A recent review on Tamiflu has shown that more than 10,000 pages of regulatory evidence were not enough to clarify major discrepancies regarding the effects and mode of action of the drug, the authors said.
In the course of trying to get hold of the regulatory evidence, the authors received several explanations from the manufacturer, Roche, as to why it would not share its data.
“It’s been very frustrating,” Professor Del Mar said. “Roche has been stalling us basically. You can speculate why. Some of our analyses seem to suggest Tamiflu doesn’t work in the way everyone thinks it does. It may work in odd ways.”
In their paper, the authors write: “It is the public who take and pay for approved drugs, and therefore the public should have access to complete information about those drugs. We should also not lose sight of the fact that clinical trials are experiments conducted on humans that carry an assumption of contributing to medical knowledge.
"Non-disclosure of complete trial results undermines the philanthropy of human participants and sets back the pursuit of knowledge.”
Industry and regulators have historically treated clinical study reports as confidential documents, blocking scrutiny by independent researchers, the authors said.
In a response published in the same journal, representatives from drug regulators in England, France and The Netherlands argue that “potential benefits for public health of independent (re)analysis of data are not disputed and, in an open society, trial sponsors and regulators do not have a monopoly on analysing and assessing drug trial results. Yet, the different responsibilities of regulators and independent analysts have to be acknowledged.”
They argue that publishing all trial data could pose a threat to patient confidentiality, and point out that so-called independent analysis does not remove the potential for conflict of interest.
“Personal advancement in academia, confirmation of previously defended positions, or simply raising one’s own visibility within the scientific community may be powerful motivators.”
But Professor Del Mar said the regulators had “set up a kind of straw dog to knock over here. Patient confidentiality is paramount, of course … but we’re after clinical study reports, and they don’t have individual patient data.
"As far as conflicts of interest go - in every endeavour in science, people come at hypotheses they want to test with some baggage on board. That’s true of everything. The whole scientific method consists of establishing a hypothesis and then testing, and that which doesn’t fall over is then regarded as the truth, for the moment.”