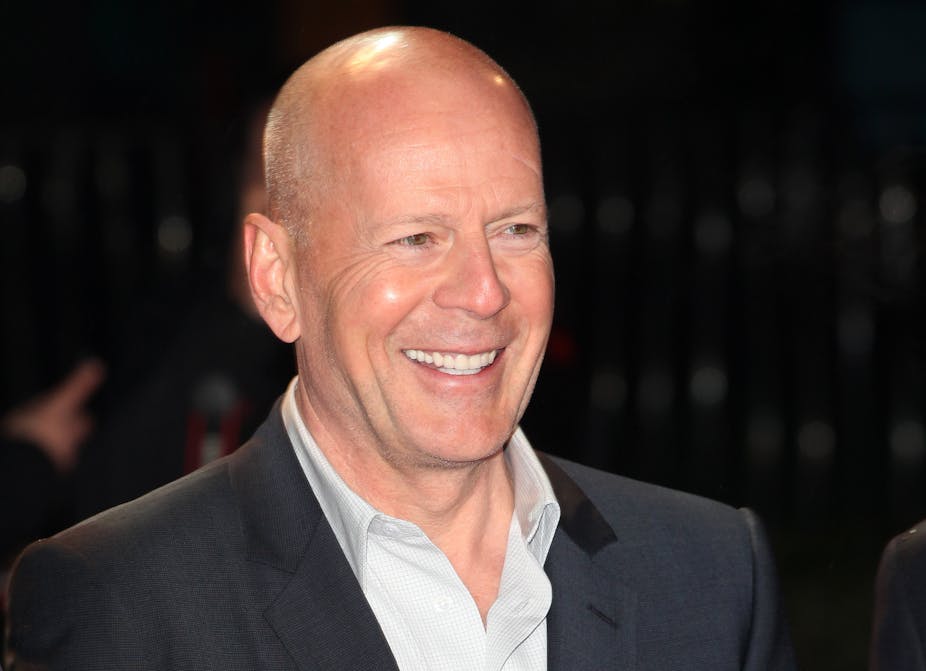
Few people had probably heard of frontotemporal dementia until earlier this year, when the family of actor Bruce Willis announced the 68-year-old had been diagnosed with the condition.
Frontotemporal dementia is a rare disease – thought to account for only one in every 20 cases of dementia. Symptoms usually develop in a person’s late 50s, first affecting their behaviour, personality and language ability. Unlike other forms of dementia, memory only becomes impaired in the late stages of the disease.
People diagnosed with frontotemporal dementia usually die within eight years of their diagnosis. While around 30% of cases are inherited, the cause of frontotemporal dementia is largely unknown. This also means there are no cures available or treatments to slow its progression.
But recent research, I have published with colleagues at Lund University, may have brought us one step closer in our understanding of how frontotemporal dementia develops and progresses. We discovered that the way your brain looks may determine your resilience to the condition.
Brain folds
During pregnancy, as a foetus’s brain grows within the womb, it develops its distinctive folds while expanding within the skull. These brain folds play an important role in our later cognitive function.
The folds that form early in foetal development are found in both sides of the brain in every person. But there’s one fold that sometimes develops later on in the process. It’s called the paracingulate sulcus – and not everyone has it. In those that do have it, it can either be present on just one side of the brain or both sides.
The paracingulate sulcus is interesting, as its presence can make a significant difference to cognitive ability. For example, research has shown that people with a left but not a right paracingulate sulcus have a cognitive advantage – performing better on tasks involving control and even memory.
Given the link between the paracingulate sulcus and cognitive function, our research team at Lund University – alongside colleagues in the US and Amsterdam – began studying this brain fold’s role in dementia.
To really understand what role the paracingulate sulcus plays, the team decided to focus on a type of dementia where brain damage occurs in the same region as this brain fold. The obvious choice for this research was frontotemporal dementia. This aggressive form of early-onset dementia primarily attacks the frontal lobes of the brain – particularly the central portions surrounding the paracingulate sulcus.

Our team studied MRI brain images of 186 people who had been diagnosed with frontotemporal dementia. We excluded participants who had frontotemporal dementia with a genetic cause. Around 57% of participants had a paracingulate sulcus on the right side of their brain.
We discovered that in participants who had this extra fold on the right side of their brain, their dementia symptoms began on average two and a half years later. This might mean that the paracingulate sulcus may delay the onset of symptoms. These findings were statistically significant – showing they weren’t due to chance or other factors.
This two-and-a-half-year delay in symptoms may not sound like much, but considering the poor prognosis of the condition and the burden of symptoms, this is an extremely meaningful amount of time for patients and their relatives.
Cognitive reserve
That said, after the symptoms do begin, patients with this extra brain fold became sicker at a faster rate and survived for a shorter length of time than patients who do not have the fold. So despite the delay in symptoms, patients with and without this extra brain fold still died at a similar age.
Although it may sound strange that a factor can both delay symptoms and later speed them up, this paradox is a key feature of a principle referred to in neuroscience as “brain reserve”. Brain reserve describes a structure in the brain which provides resilience to a disease before symptoms develop.
Critically, there becomes a point at which the disease overcomes these protective mechanisms, and the patient develops symptoms. After this critical point, people with high brain reserve decline rapidly – faster than people with low brain reserve.
For example, high brain reserve explains why Alzheimer’s disease starts later in highly educated people – though the disease progresses faster for them when symptoms start. According to our research, the paracingulate sulcus operates by a similar principle – first protecting people from symptoms, then progressing rapidly when symptoms do start.
Our research is the first to identify a protective structure in the brain which delays the onset of symptoms in people with frontotemporal dementia. If we can now uncover a way of preserving this protective quality, it could lead to the development of treatments which can help keep symptoms – and the disease – at bay.