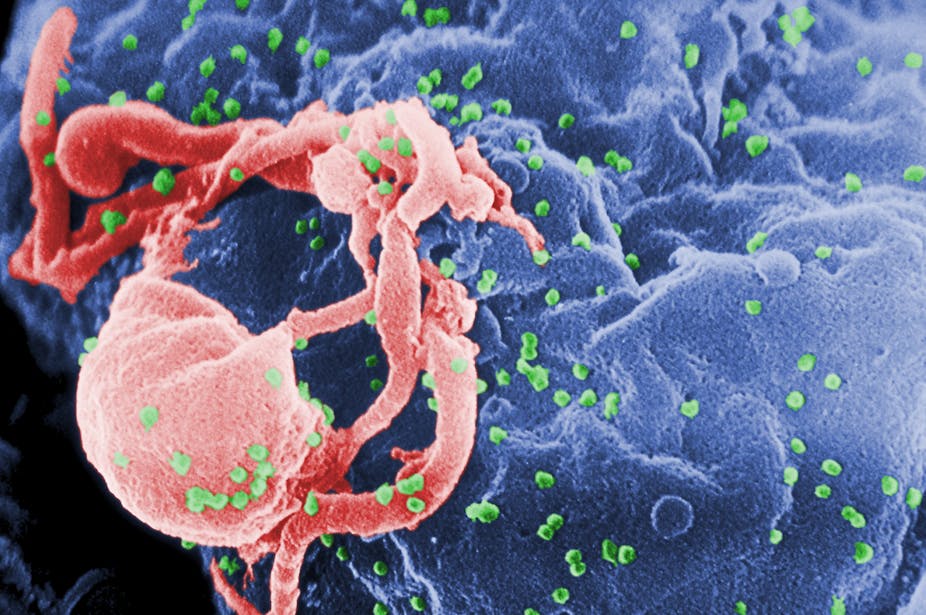
Despite three decades of research, an HIV vaccine remains elusive. The main reason for this is the virus’s uncanny ability to evolve resistance to immune control, so understanding how the virus adapts to the earliest immune responses is critical for success. Recent work involving computer simulation provides some insight into the problem we face.
Most infections by human immunodeficiency virus type 1 (HIV-1) are thought to be established by a single virus particle or genome. This means the viral population infecting a patient starts with virtually no genetic variation whatsoever. And without genetic variation, there’s no scope for evolution. That’s why the extremely rapid adaptation of the virus to the earliest immune responses is so puzzling.
How does the virus do it?
In the most recent issue of Genetics, I report on an investigation into the evolutionary dynamics behind HIV’s rapid adaptation.
I used a mathematical model of a virus population infecting a patient coded into a computer program to simulate viral evolution. The model includes only those components of the system that are thought to be critical to understanding the phenomenon.
In this case, the most important of these parameters are the number of viral protein regions targeted by the immune system; the rate of killing of infected host cells by the earliest immune responses; the rate of mutation of viral genes; the rate of viral genetic recombination; and the size of the viral population.
The emergence of new viral genetic variants, due to mutation and recombination, and changes in their frequencies (because of natural selection by the immune system and random effects of a finite population size) were then tracked across generations of the virus. Changing the values of the parameters in the model allowed me to analyse their influence on HIV’s adaptive dynamics.
Because HIV has been the focus of so much research, the values for the important parameters in the model are fairly well established. By varying these values to account for uncertainty, we can ask – is it realistic that a virus population that started from a single genome adapts to the earliest immune responses at the phenomenal average rate of one amino acid change every 22 days? To answer this question some complexities had to be addressed.
Engaging with complexities
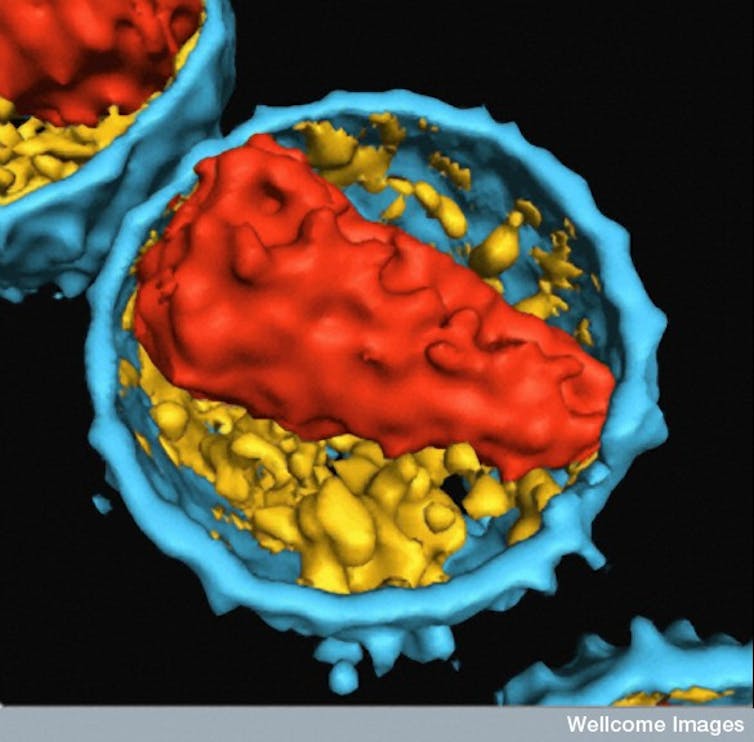
First, what is the size of the viral population infecting a patient? This is critical: adaptation occurs more rapidly in large populations because there are more genomes to mutate and fewer random sampling effects on the frequencies of genetic variants than in small populations.
In a typical patient, there are about ten million infected cells producing a total of about ten billion virus particles every day. But only a small fraction of infected cells are capable of producing infectious virus particles, and it’s the size of this much smaller “breeding population” that’s important.
Second, how much interference is there among mutations beneficial to the virus? Mutations arise simply by random errors introduced during the copying of the genome in one step in the viral life cycle. If, by chance, a mutation produces a change in a protein that prevents the immune system from detecting the virus, then the genome carrying this “escape mutation” will leave more copies in the next generation than genomes without the mutation.
By this deceptively simple mechanism (natural selection), escape mutations may become more common in the viral population over time. But a complication arises if the immune system targets different viral proteins at the same time, causing different genomes carrying different escape mutations to spread in the population simultaneously.
This should slow down the overall rate of adaptation as these genomes compete with each other for prominence in the population. But how likely is this to occur in HIV?
Extreme conditions
Simulations showed the establishment of a viral population by a single genome results in a small effective population size of about 1,000 infected cells by early chronic infection. This translates into low background genetic variation throughout early infection.
Under these conditions, the dynamics of adaptation are most sensitive to the mutation rate and the number of protein regions targeted simultaneously by the immune system. And both parameters required values at the high ends of their plausible ranges to permit enough beneficial mutations to arise. For example, the immune system had to target five viral protein regions simultaneously, the maximum number reported.
Interestingly, although a high number of protein regions were targeted, there was little evidence of interference between escape mutations. This is because the effective population size is so small that, even with a high mutation rate, individual escape mutations tend to arise and spread sequentially rather than simultaneously.
The upshot of this is that, with realistic parameter values that allow rapid adaptive evolution, the virus is able to evolve at the high rate observed even if the infection is established by only one genome.
Implications
An important implication is that designing vaccines that direct the immune system to the usual viral protein targets is likely to fail because the virus is able to evolve so readily in response, even in early infection when it’s most vulnerable. In fact, this approach may be counter-productive since focusing the immune system’s resources on specific protein regions may make it easier for the virus to adapt.
A solution that’s often suggested is to target protein regions that are strongly constrained - those where escape mutations would severely reduce HIV’s ability to replicate. But even this strategy may not be successful since secondary mutations that compensate for such decreases in fitness may be common.
Clearly, there’s no simple solution to this problem. If we are to devise effective vaccines, we must improve our understanding of HIV’s adaptive evolution.