Circumcision is the oldest and most frequent surgical procedure in the world. In some cultures, it marks a clear break from childhood to adulthood. But, reports of young men dying during traditional initiation rites due to spontaneous bleeding are devastating. The Conversation Africa’s Health and Medicine Editor Joy Wanja Muraya asked Dr Peter Kibet Shikuku for his views on a safe circumcision programme in Kenya for boys with haemophilia – a bleeding disorder.
How prevalent is haemophilia in Kenya?
Most patients with haemophilia are born with it, congenital, while others acquire it.
Patients must see a specialist, a haematologist, before any surgery to control their bleeding. While circumcision is not a major operation, it can lead to death because the bleeding is slow, consistent, continuous and prolonged.
The prevalence of haemophilia is the same in all communities and remains at 1 per 10,000 in any population. As a country we have only reached awareness of the disease at 14% of those affected.
Superstitions are driven by lack of awareness in the communities forcing some parents to hide or lock away their children from the general public due to associations of the condition with bad omen.
During circumcision by traditional healers, the injured young men and those slow to heal are abandoned in the forest to die. Circumcision, they say, is not for weaklings.
How different is circumcision for haemophiliacs?
Circumcision carries different meanings in Africa and globally. In most communities in Kenya, it’s a rite of passage practiced by most communities on boys and/or girls.
It involves either the removal of certain teeth, tattooing parts of the body, piercing of earlobes, removal of the foreskin or a combination of practices.
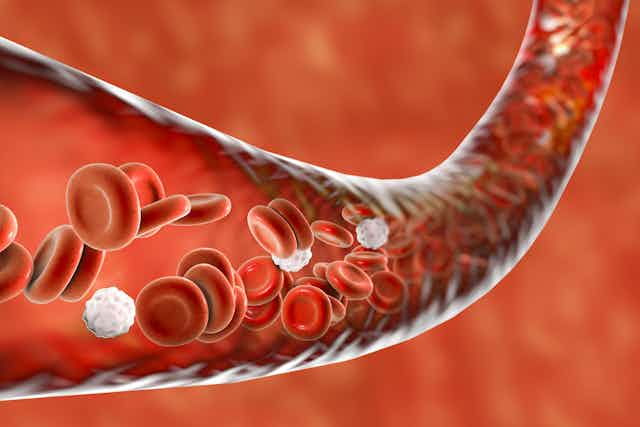
During these rites blood is lost, with a few complications occurring. But, some young men die due to lack of adequate testing for haemophilia - a genetic disorder that impairs the body’s ability to make blood clots.
This is complicated by lack of information within the circumcising communities on the bleeding disorder. The uninitiated are often stigmatised, ridiculed and bullied by their peers.
Because of this, some young men do not disclose that they’re haemophiliac and undergo circumcision without the precautionary measures, leading to complications, and even death.
Blood clot elements that manage haemophilia during circumcision are not readily available and are expensive. The missing factor protein is injected into the affected person’s vein enabling the body to continue the clotting and hence stop the bleeding.
First case study
A 23 year old man in high school was under peer pressure to get circumcised. They threatened to forcibly circumcise him themselves. He knew he had haemophilia and needed the factor concentrate.
He travelled from one health facility to another to accumulate enough of the concentrate . But, it wasn’t enough and he was circumcised with these expired products in one of the health facilities.
He developed antibodies to factor eight on the fifth day after the operation and ended up with a by passing agent to overcome the antibodies till he healed. It’s not even possible to establish the reason behind antibody development in this patient.
Second case study
A young man in his 20’s with haemophilia had suicidal tendencies. Being “uncut” was unacceptable and demeaning in his community.
He got clinicians to take him through the procedure even though they had very limited resources. A group of consultants decided to use blood components, a few factor concentrates and tranexamic acid. This combination worked despite the shortcomings associated with it. He recovered and is now one of Kenya’s paralympic sportsmen.
What strategies and technologies are used to ensure safer circumcision amongst haemophiliacs?
There are 450 young men attending the haemophilia comprehensive care clinic at Kenyatta National Hospital and Moi Teaching and Referral Hospital. They make up about 10% of all haemophiliacs countrywide.
Most of them are not circumcised despite coming from circumcising communities, because of haemophilia. That is because of the lack of factor concentrates which are essential in preventing bleeding.
At Kenyatta National Hospital, circumcision was the least of procedures to be offered to haemophiliacs due to lack of factor concentrates. The clinical team opted to use tranexamic acid alternating it with cryoprecipitate to stop heavy bleeding, commonly used in peripheral facilities by uninformed surgeons.
This seemed to have worked though in case of any inhibitor development, there were almost no alternative treatment and fatalities were almost the norm.
Towards the end of 2015, Kenya Hemophilia Association initiated a “safe” circumcision programme in the two health facilities, that has led to circumcision of about 30 haemophilia patients. All the young men were prepared before the surgery by getting clotting factors and later followed up in the wards until they got fully healed.
What challenges do you face running this safer circumcision programme? What lessons have you learnt?
The lack of cost effective drugs to manage patients during circumcision is the most urgent concern.
The shortage of factor concentrates in public hospitals and clinics forces us to rely heavily on donations from the World Federation of Haemophilia. The availability of the concentrates in select health facilities locks out families with haemophiliac young men from safe circumcision.
Since the safe circumcision programme started, parents are bringing their sons for registration. This has enabled the programme to schedule with the surgeons all procedures annually.
We are creating public awareness of the signs and symptoms associated with the disease so that people can seek help early, before the young men reach circumcision age.
For young men who wish to keep to their cultural initiation rites, we have trained nurses to deliver the clotting factors at the village during circumcision supported by the traditional surgeons, elders and other decision makers.
Overall, fewer cases are now being brought to the hospital as emergencies following circumcision as compared to before. The programme intends to determine the best protocol which is cost effective and easily implemented at the lower health facilities in the counties.