The trouble with treating cancer is that each type has its own quirks. The quirks of pancreatic cancer make it one of the most lethal. The survival period after diagnosis is only four to six months. The main reason is that treatment with drugs – chemotherapy – which has had some success in extending lives for patients with other cancers, fails in the case of pancreatic cancer.
The widely believed reason for this failure has been that in pancreatic cancer, the tissue that surrounds the tumour, called the stroma, blocks the delivery of chemotherapy drugs to the tumour. A new study, published in Cancer Cell, questions that logic. It shows that the stroma, instead of supporting tumour progression, inhibits it by activating body’s immune system’s attack on the tumour.
Tumorous tale
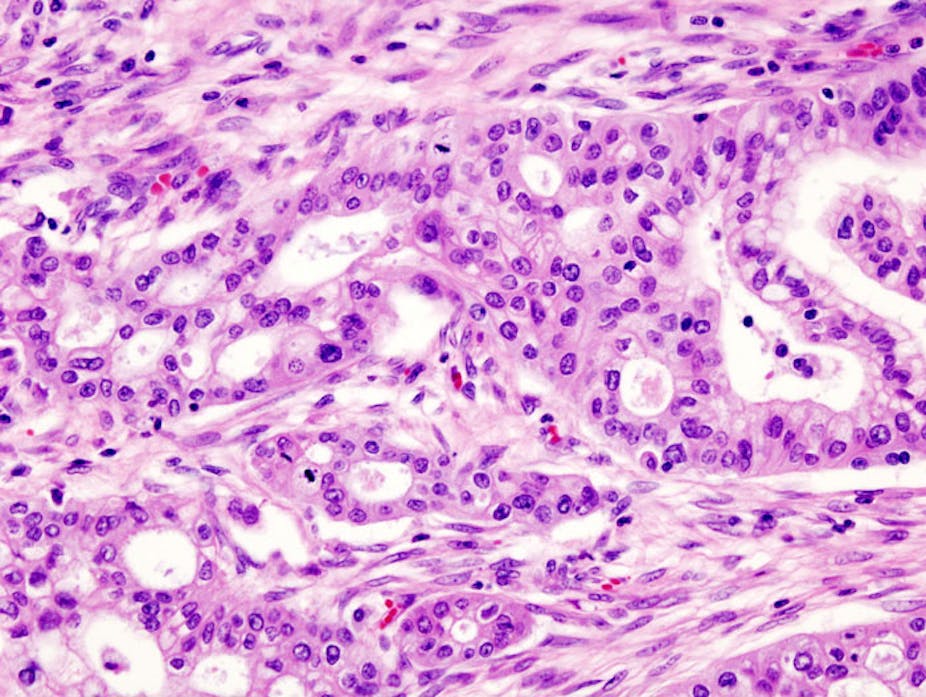
All tumours are composed of some cancer cells and mostly stroma. But pancreatic cancer is unique – only around 10% of the cells in the tumour are cancer cells. That is the least proportion among all cancer types. The remaining 90% is the stroma consisting of special cells known as myofibroblasts.
Taking clues from this distinctive property of pancreatic cancer, previous studies indicated that stroma can act as a physical barrier to the chemotherapy drugs. This finding created a slew of clinical trials for combining chemotherapy with “stromal depletion therapy” – that is, removing the stroma from the tumour. However, these trials had to be stopped abruptly when patients receiving this combination therapy were found to have an accelerated tumour progression as compared to those that only received chemotherapy. The reasons for this disappointing result remained unclear.
Now, in the new study, Raghu Kalluri and his colleagues at MD Anderson Cancer Center have perhaps found the reason. They propose a mechanism underlying the failure of the clinical trials.
Using mice, who act as proxy for humans, Kalluri and colleagues show that the depletion of myofibroblasts – the major component of stroma – at any stage of pancreatic cancer does not improve the efficiency of chemotherapy. Instead tumours grow more aggressively. This leads to making it difficult for the immune system to control cancer and eventually to higher number of mice deaths. This indicated to Kalluri that perhaps the stroma is inhibiting the tumour instead of promoting.
“We did these experiments thinking that we would show the importance of myofibroblasts and fibrosis in pancreas cancer progression, but the results went completely against that hypothesis,” Kalluri said in a statement.
“This supportive tissue that is abundant in pancreatic cancer tumours is not a traitor as we thought but rather an ally that is fighting to the end. It’s a losing battle with cancer cells, but progression is much faster without their constant resistance. It is like having a car with weak yet functioning brakes vs having one with no brakes.”
Dump me not just yet
It is not all bad news for stromal depletion therapy, however. Kalluri found that tumours with less stroma had higher levels of CTLA-4, a protein which is responsible for shutting down the immune system response. When these tumours were treated with ipilumimab, a drug that blocks CTLA-4, survival time of the mice increased by 60% as compared to that of the untreated control mice.
This is a shot in the arm for cancer immunotherapy – therapies that enable the body’s immune system to fight cancer directly – which has been considered as the Breakthrough of the Year 2013 by the journal Science. This sort of therapy might be more effective for pancreatic cancer patients with relatively less stroma in their tumours. Or a combination of immunotherapy and stromal depletion therapy might be more effective for pancreatic cancer patients with dense stroma, which is usually the case.
The development offers hope for a disease in which only seven out of 100 patients survive for five years after being diagnosed. For managing pancreatic cancer treatment better, rapid progress in its earlier diagnosis is essential.