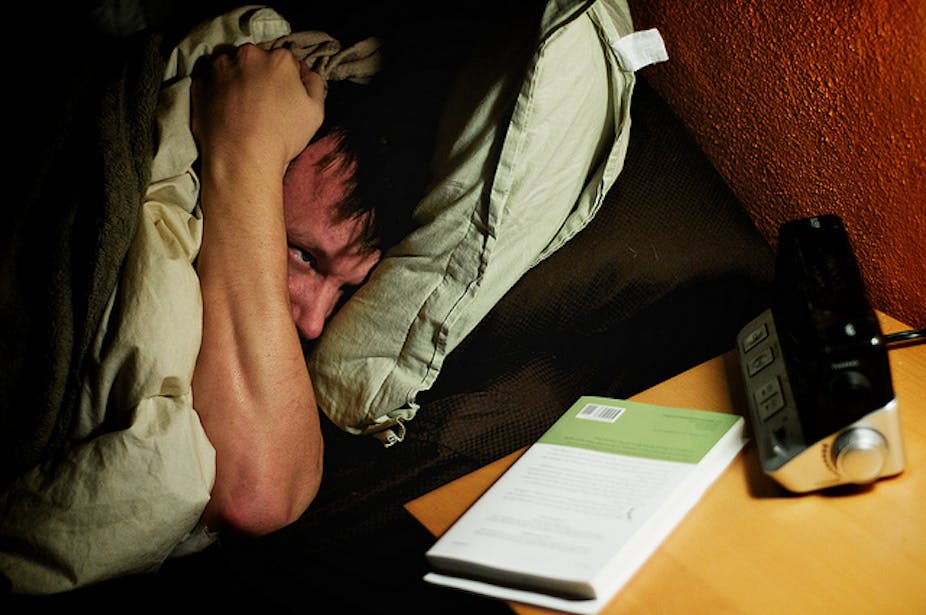
People with three insomnia symptoms have a three-fold higher risk of heart failure than people with no insomnia, a large study has found, but the researchers stopped short of saying sleep problems caused heart failure.
Insomnia symptoms include trouble falling asleep, problems staying asleep, and not waking up feeling refreshed in the morning.
Heart failure occurs when the heart muscle has become so weak or stiff, it is unable to pump blood properly around the body.
The Norweigian study, published today in the European Heart Journal, analysed data on 54,279 people aged between 20 and 89 for an average of more than 11 years.
“We found that persons suffering from insomnia have increased risk of having heart failure. Those reporting suffering from all three insomnia symptoms simultaneously were at considerably higher risk than those who had no symptoms or only one or two symptoms,” said lead author Dr Lars Laugsand, a post-doctoral fellow in the Department of Public Health, Norwegian University of Science and Technology in Norway.
“We do not know whether heart failure is really caused by insomnia, but if it is, insomnia is a potentially treatable condition using strategies such as following simple recommendations concerning sleeping habits (often referred to as sleep hygiene), and several psychological and pharmacological therapies.”
Dr Laugsand said evaluation of sleep problems might provide additional information that could be used in prevention of heart failure.
The researchers relied on information on insomnia provided by participants, who all came from the Nord-Trøndelag County in Norway, as well as heart failure data from hospitals and the National Cause of Death Registry.
The subjects, 97% of whom were Caucasian, were mostly representative of Norway but with a slightly lower average education and income levels than the rest of the country.
The researchers excluded those who had already experienced heart failure before the study began.
The researchers adjusted for age, sex, marital status, education, shift work, blood pressure, cholesterol, diabetes, body mass index, physical activity, smoking, alcohol, any previous heart attack, depression and anxiety.
Professor Leon Lack, a sleep expert and professor of Psychology at Flinders University said some chronic insomniacs had elevated levels of the stress hormone cortisol.
“Chronic insomniacs are clearly distressed by their situation and have worry or frustration about their poor sleep. That could be a mechanism that is predisposing them for increased risk of heart failure later on,” said Professor Lack, who was not involved in the Norwegian study.
“Any little variable [the researchers] were not able to control for could be a contributing factor. My concern is that this information just reinforces the concerns insomniacs have. Many of them believe they are going to have medical problems as a result of their insomnia and that is a contributing worry or anxiety which exacerbates the insomnia.”
In comments released by the UK Science Media Centre, Professor Emeritus Alun Evans, Visiting Senior Research Fellow at the Centre for Public Health at the Queen’s University of Belfast, said the study was huge and well-conducted and demonstrated “a very significant association between the number of symptoms of poor sleep at baseline and the development of heart failure a decade later.”
“Could this association be causal? Links between sleep disturbances or deprivation and childhood overweight and learning impairment, and adult obesity, diabetes, cancer, heart disease, and cognitive dysfunction have been reported previously. How might these diverse conditions be linked?” he said.
Dr Tim Chico, Senior Clinical Lecturer and honorary Consultant Cardiologist at the University of Sheffield/Sheffield Teaching Hospitals, said heart failure symptoms include shortness of breath, tiredness, ankle swelling and distension of the abdomen.
“Our ability to treat heart failure has improved massively in the last few years, with many hospitals setting up specific heart failure clinics and services. Diagnosis of heart failure usually involves an ultrasound scan of the heart, blood tests and an assessment by a specialist,” he said.
“This is an ‘association study’; it links insomnia to heart failure, but does not prove that insomnia causes heart failure or vice versa. Studies like this raise interesting suggestions that need further work to examine,” said Dr Chico.
“Insomnia is a very unpleasant condition, but there are effective lifestyle changes that can reduce it, such as weight loss and exercise. Luckily, many of the things that reduce the chance of heart failure also reduce insomnia; good diet, exercise, weight loss and not smoking.”