About 6,000 years ago, a bacterium underwent a few genetic changes. These allowed it to expand its habitat from the guts of mice to that of fleas. Such changes happen all the time, but in this particular instance the transformation eventually resulted in the Black Death that wiped out a third of Europe’s population in the 14th century.
Yersinia pestis (YP), which causes plague, evolved from an ancestral bacteria called Yersinia pseudotuberculosis (YPT). This happened somewhere in China, from where it spread westward causing disease in both animals and humans. In a new study, published in the journal Cell Host & Microbe, researchers at the National Institute of Allergy and Infectious Diseases have retraced the genetic changes that enabled this bug to become one of the most feared microbes.
Making the switch
Infections due to both YPT and YP are classified as “zoonoses”, transmissible from animals (mainly rodents) to other animals, including humans. YPT is transmitted by fecal contamination of food and water. In contrast, the more lethal YP is transmitted via bites of infected fleas.
Genetically, YP possesses a smaller subset of the genes present than its ancestor YPT. And yet, while YPT causes a relatively mild disease in various mammals, YP causes types of plague – a severe, inflammatory disease that may be fatal if left untreated.
When a microbe evolves into a more potent agent of disease, the usual reason is the addition of genes (for example, genes that make a bug resistant to antibiotics). But, according to Yi-Cheng Sun and colleagues, the YPT-to-YP switch involved both addition and removal of genes, resulting in a net loss.
Sometimes, a microbe in a given environmental niche undergoes changes in its genetic make-up. These changes come in four types:
- neutral – has no effect
- deleterious – renders the surrounding environment inhospitable, causing it to die or move to a new niche
- allows adaptation – minor change to suit the new environment
- increase fitness – confers the ability to exploit the new niche to thrive
Adaptive genetic changes (such as numbers 3 and 4) may thus establish a new habitat for the organism, and may lead to the emergence of a new species. Ecologists call this process adaptive radiation. However, not all the key genetic mechanisms involved in this process are currently well-understood.
Nonetheless, adaptive radiation likely explains the changes YP underwent to become highly infectious. Sun and colleagues present convincing evidence that adaptive genetic changes in YP – involving the loss of three genes and gain of one – allowed it to thrive in the flea internal environment as compared to YPT.
YPT, ingested by a rodent, lives peacefully in its gut, until there are enough of its brethren or the host’s immunity falls. When that happens, YPT slips into the rodent’s bloodstream. Fleas, living on the rodent, happily suck in the bug-laden rodent blood. Inside the flea, a sticky protein that YPT makes allows it to set up home in the hindgut (lower digestive tract) without causing disease. It is then regularly shed through the flea’s feces.
Flea master
YP lacks the ability to make that sticky protein. This means that it cannot live in the hindgut like YPT. Interestingly, the only gene YP gained allows it to sit instead in the midgut and foregut of the flea, closer to the mouth.
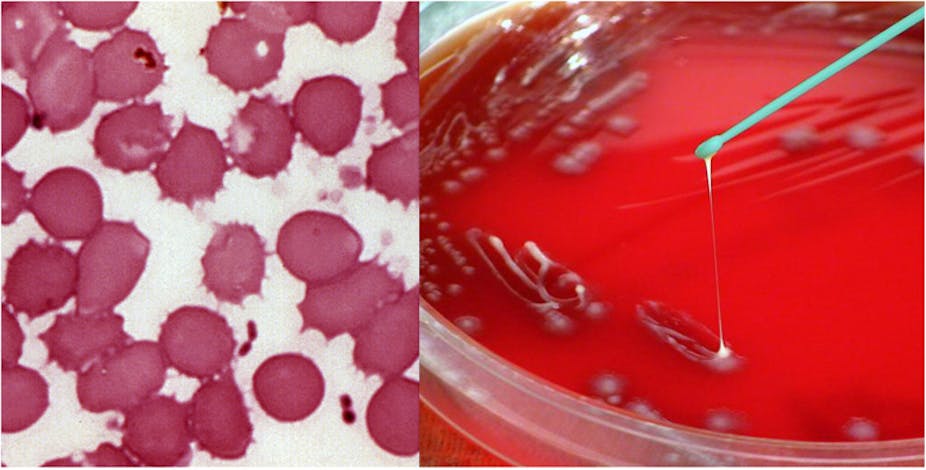
YP is able to do this by covering the flea gut surfaces with a polymeric biofilm in which it remains embedded. YPT cannot do this because three genes suppress this ability. Incidentally, these are the three that YP lost, thereby gaining this function. The biofilm allows YP to remain in the flea (when YPT is removed with feces). This, along with the gut positioning, increases YP’s chances of transmission to a new host via flea-bite.
YP infection – via rodent hosts and flea transmission – continues to occur sporadically in some parts of the world, such as Africa, Western South America, the Western United States, and parts of Asia. But there is evidence that YP may be losing further genes, reducing its disease-causing potential. Besides, modern antibiotics can treat such plague-type infections.
Next, read this: Study finds widespread antibiotic resistance in nature