The deadly second wave of coronavirus infections in India over the past few weeks has led to a sharp spike in deaths and overwhelmed the health system. Increasingly higher demand for healthcare has outstripped available hospital beds, oxygen, ambulances, drugs and healthcare workers.
Several experts have pointed out that the Indian healthcare system, dominated by the private sector, has not been adequately prepared to deal with such a massive crisis. The Indian government needs to prioritise reform measures that address these shortcomings to avoid a similar crisis in the future. This includes increasing spending on the health sector, ensuring a stable supply of trained workforce and essential medicines, and collecting reliable data on key health indicators.
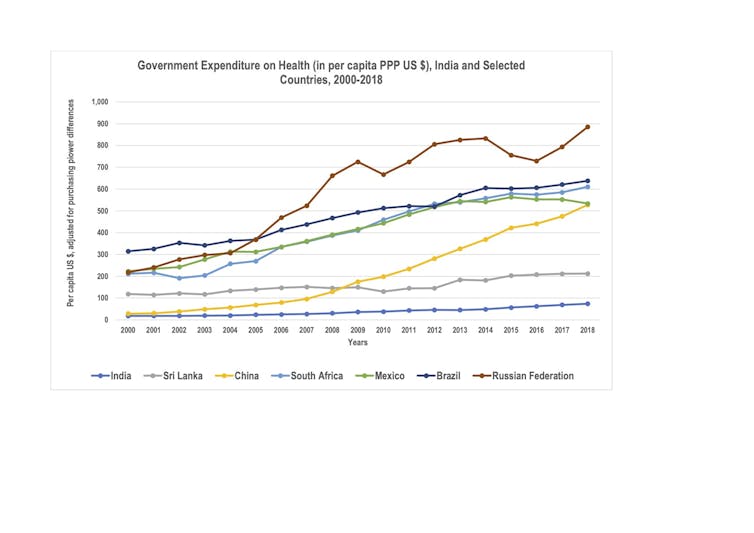
Among countries with a similar level of income and economic growth, India spends very little on health. Despite being the sixth-largest economy in the world, India spent a paltry 3.5% of its GDP (in 2018) on health. By comparison, Brazil spent 9.5% of its GDP on health, China and Mexico 5.4%, and the UK 10%.
Most of the money spent on health in India comes directly out of people’s own pockets, with government spending on health being one of the lowest in the world, averaging about US$38 per person per year over the past two decades.
Per capita spending on healthcare
India’s hospitals are mostly concentrated in cities, and primary healthcare is weak in both urban and rural areas. The lack of critical healthcare infrastructure in government health facilities in most parts of the country means it is ill-prepared to meet routine demand, let alone crises.
Long-standing demands from experts and academic researchers, and even time-bound commitments from the national Ministry of Finance and in the National Health Policy for increasing government expenditure on health to 2.5-3% of GDP have so far met with few concrete results.
More investment is also needed for expanding capacities for scientific research across different disciplines of healthcare in the country. Stable public funding and incubating a strong cadre of research professionals go a long way to improving preparedness and ensuring a swift response to any crisis.
India’s healthcare system suffers from a massive shortage of trained health workers: doctors as well as paramedical staff, such as nurses and laboratory technicians. Apart from poor salaries and working conditions in the public hospitals and clinics, the limited availability of medical and paramedical education and training facilities across the country is a major constraint. A recent expansion of medical schools, mostly in the private sector, has fallen short of the growing demand.
Massive growth of medical and paramedical training facilities is needed to help bridge the gap. And the expansion must be prioritised in under-served regions, such as rural areas and smaller towns in poorer states, where the shortfalls are most pronounced.
Unaffordable drugs
India is a world leader in the production of drugs and vaccines, and often referred to as “pharmacy of the world”. But prices of most medicines, including essential medicines, is unaffordable for the average citizen. As spending on drugs account for a large share of the healthcare expenses for Indians and is a major cause of financial distress, pricing and quality reforms in the pharmaceutical sector are essential.
This should address unfair practices, such as highly differential pricing for similar pharmaceutical compounds, and tackle the sale of counterfeit drugs. Also, there is an urgent need to improve drug procurement and distribution policies for public facilities to ensure the availability of essential drugs. Examples, such as in the province of Tamil Nadu, where drugs are purchased and distributed across public health facilities through a transparent, technology-supported system, are worth considering.
Better data, better governance
India’s existing systems to collect, process and monitor crucial information of public health and healthcare indicators are weak and often non-existent, duplicated and of doubtful quality. Dismantling these archaic systems and establishing an integrated, robust and transparent health information system in India is fundamental to any reforms. The reliable, timely flow of information across different levels of the healthcare system, harnessing recent advances in big data and mobile technology, can significantly improve preparedness and responses to any future crises.
Combating public health challenges in a country of India’s size, population and regional variations critically hinges on the quality of governance and local capacities. This requires transferring greater power to provincial and local governments in deciding priorities, use of resources and managing health facilities. Past attempts in doing so through reforms aimed to decentralise health system planning and administration under the National Health Missions have had limited success, largely because of poor funding and inadequate investments in building required skills among the responsible officials. Strengthening local governance in the health sector needs to be the bedrock of any future reforms.

