It’s almost exactly two years since the emergence of the swine flu virus was announced by the World Health Organisation (WHO). This was the first flu pandemic in 41 years and the start of another flu season provides a good juncture to look back at how we handled it.
The most remarkable thing about the pandemic in 2009 was how fast the virus spread around the world. Within a few weeks of its detection, it had already reached all the continents.
The pandemic alert came via the World Health Organisation (WHO) following a report from Mexico of serious influenza-like illness and work done by the United States Centers for Disease Control and Prevention (CDC)
CDC undertook the genetic sequencing of a virus that had infected two children in California. Swine flu was not unknown in the United States, with people occasionally reporting symptoms after visiting fairs and farms. But, this time, CDC discovered that this was a novel strain.
They found it was not like those that usually infected people and notified the WHO. When it was shown that the same novel virus was responsible for the outbreaks in Mexico, WHO issued a major worldwide alert.
The WHO Collaborating Centre for Reference and Research on Influenza at the Victorian Infectious Diseases Reference Laboratory (VIDRL) in Melbourne is one of the five international centres of the WHO Global Influenza Surveillance Network (GISN).
The Centre was notified about the new swine flu virus on Anzac Day. The first cases to be confirmed by the Centre were from a high school group in Auckland.
They had been on a trip to Mexico and returned via California, and some had symptoms of influenza on the flight home. We knew they carried the pandemic virus by April 28.
This group was a typical example of how people helped the virus spread - travelling by plane, it reached all continents extremely rapidly.
Future pandemic viruses will likely spread in a similar manner.
A virus’s spread is quicker when most people don’t have any immunity against it and this was the case during the swine flu pandemic.
We all develop some immunity against the seasonal flu as we are repeatedly exposed to various strains throughout our lives.
Interestingly, the only group that seemed to have any cross-protection during the swine flu pandemic were older people, especially those born before 1930.
This is because the swine flu virus looks more like the 1918 Spanish flu pandemic virus to our immune system than the viruses that have been circulating since.
It is suspected that relatives of the 1918 virus had been circulating among pigs and possibly other animals since before that outbreak.
Since evolution of viruses in animals is slower than that in humans, the seasonal flu viruses that were descended from the 1918 pandemic virus had changed considerably but those circulating in swine had not.
So, because only the very old had significant protection against it, the new virus spread quickly.
Those most affected by the swine flu were young people and it spread rapidly among school children.
The 2009 flu vaccine released before the pandemic did not protect against swine flu and immunity against the seasonal influenza viruses did not offer enough cross-protection to stop the pandemic.
The matter was further complicated by the fact that many people were asymptomatic or experienced mild symptoms. This may actually be true for the seasonal flu as well but the pandemic led to surveys of population immunity that are not usually performed.
As immunity builds in the population because of infection or vaccination, it puts pressure on the virus to evolve to escape the antibody response and leads to the emergence of a new virus strain.
This is the reason that we update seasonal influenza vaccines periodically.
To keep up with this moving target, the WHO has established a global network of influenza laboratories. The WHO Collaborating Centres for Reference and Research on Influenza receive samples sent by national laboratories around the world to monitor how flu viruses are changing.
The Centres help the WHO recommend which viruses to use in influenza vaccines and supply them to the vaccine manufacturers.
The same process took place for the pandemic vaccine and enabled vaccination campaigns to start in Australia and China in September 2009 and in many other countries soon afterwards.
Seasonal influenza vaccines now contain the swine flu virus as well as the two other influenza viruses that currently circulate in humans (H3N2 and B).
In Australia, these vaccines are available from three different pharmaceutical companies. One of the three brands caused an unusually large number of reactions in young children in 2010 and is no longer available for those under the age of 5 years.
The other two brands can be used for under-5s and all three are approved for older children and adults.
The pandemic in 2009 reminded us how difficult it is to stop the spread of a contagious respiratory virus like influenza. That is particularly so today when a virus can travel across the globe by plane within 24 hours.
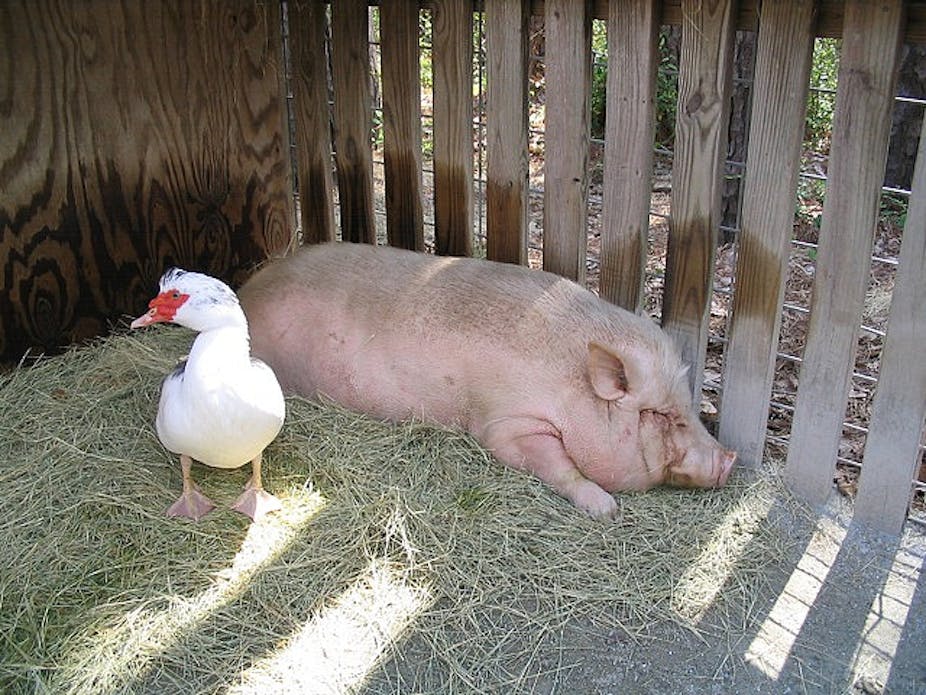
If we are to reduce the likelihood and impact of future pandemics, we need to improve virus surveillance and biosecurity in domestic pigs and poultry.
We also need better vaccines – vaccines that induce long-lasting immunity and provide cross-protection against emerging influenza viruses.
Influenza viruses
There are three types of influenza virus that can infect humans:
Type A viruses infect birds, pigs, horses and many other animals. They cause seasonal epidemics in humans. Only type A viruses cause pandemics.
Type B viruses are restricted to humans and also cause seasonal epidemics. Although they don’t cause pandemics, they do mutate, so vaccines are periodically updated to provide protection against the latest strain.
Type C viruses cause only mild disease in humans so they are not represented in current vaccines.
Mutations
The genetic material of flu viruses is in eight separate pieces and novel viruses can be formed by shuffling these pieces when two different influenza viruses infect the same cell.
A pig infected simultaneously with flu viruses from a bird and a human provides a platform for the creation of a new virus.
If the new virus can infect and spread between humans and is not blocked by our existing antibodies, it can cause a pandemic.