The Kenyan Medical Practitioners and Dentists Board has stopped the NGO Marie Stopes International from performing abortions in Kenya. Marie Stopes is a global organisation that provides contraception and safe abortion to women in urban and rural communities. Abortion is illegal in Kenya, unless a trained medical professional judges that there’s a need for emergency treatment, or that a woman’s life or health is in danger.
The Conversation Africa’s Moina Spooner spoke to Michael Mutua about the Marie Stopes ban and its implications.
How did the ban come about?
According to the Kenya Medical Practitioners and Dentists Board, they banned abortion services provided by Marie Stopes following complaints from the general public. The public claimed the organisation was running pro-choice media campaigns. These adverts specifically sought to provide women with a solution when faced with crisis pregnancies.
The adverts were also criticised by the Kenya Film Classification Board, which ordered Marie Stopes to pull them down for allegedly promoting abortion.
The Kenya Medical Practitioners and Dentists Board is the only body within the Ministry of Health that has the mandate to regulate and set policies on medical training and service provision in the public and private sectors.
Aside from closing down the abortion services, the board also ordered that Marie Stopes file all its service reports with them for two months. This is a way for them to keep track of what services the NGO is providing.
Under what circumstances are abortions legal or illegal in Kenya?
Abortion in Kenya is guided by two laws.
Kenya’s 2010 Constitution prohibits abortion unless, in the opinion of a trained health professional, there is need for emergency treatment, or the life or health of the mother is in danger. Health can refer to complete physical, mental, and social wellbeing; it’s not just related to physical factors. So factors like social pressures and the psychological and emotional distress associated with unwanted pregnancies are taken into account.
But there continues to be confusion over this for women, medical practitioners and legal bodies. That’s because, since this constitution came into effect, no policy guidelines have been created about the provision of safe legal abortion in Kenya. These guidelines would clearly define the circumstances under which the medical practitioner can do an abortion and what type of medical practitioner is authorised to perform the procedure.
These guidelines used to exist – but they were withdrawn soon after the launch of the constitution following an outcry from religious groups. The Ministry of Health also argued that the guidelines were prone to misuse by quack medics.
Without these guidelines, the older penal code law comes into effect. This law practically criminalises the act of seeking or securing abortion. It is harsher on the service provider than on the woman who terminates a pregnancy. The law can penalise the service provider with up to 14 years in jail. The patient can get seven years.
The penal code does allow surgical intervention when the life of the mother is in danger. But this is very invasive and doesn’t accommodate improved procedures like manual vacuum aspiration and medical abortion.
How many abortions happen in Kenya every year, and how?
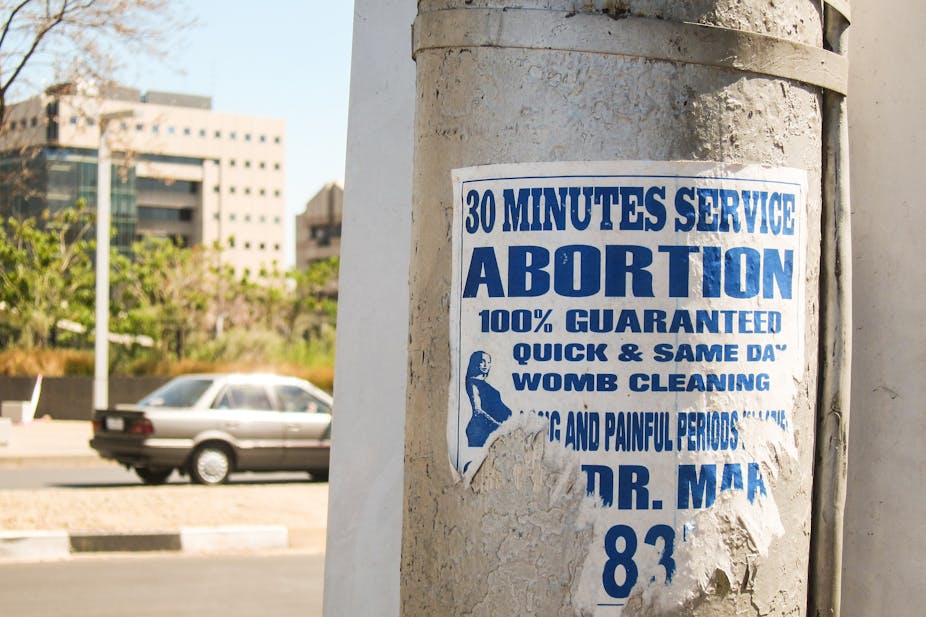
The impact of these laws means that women often turn to backstreet clinics and unsafe abortion services. Abortion is highly stigmatised within communities and at health facilities so women prefer to take a risk to assure their privacy.
A recent study by the Ministry of Health, in conjunction with the African Population and Health Research Center, revealed that about 465,000 unsafe abortions take place in Kenya every year.
As a result, nearly 120,000 women are treated in health facilities each year for complications arising from unsafe abortions. These include incomplete abortion, infection, excessive bleeding and injury to the internal organs.
The risk of maternal mortality is high. Over 77% of these cases presented are “moderate or severe” and the women are at a high risk of death.
What will the impact of the ban be?
Each year the government spends over US$5million to treat women in government facilities who have complications from unsafe abortion. This cost is high. But it’s actually an underestimation: it excludes social costs – like the loss of working hours – and out-of-pocket expenses covered by the patient or their friends and relatives.
Non-governmental players – like Marie Stopes – that provide safe abortions make a significant contribution in preventing the risks of maternal morbidity and mortality. One of the main roles they play is in preventing unintended pregnancies by providing contraception.
These organisations also provide quality counselling to patients who intend to secure abortion. However some patients, given their social situations and because of the stigma of an unintended pregnancy, will resort to unsafe abortion when safe options aren’t available.
I anticipate that by curtailing safe abortion services, without a commensurate investment in the prevention of unintended pregnancies, there will be an increase in the incidence and magnitude of complications from unsafe abortion in Kenya.