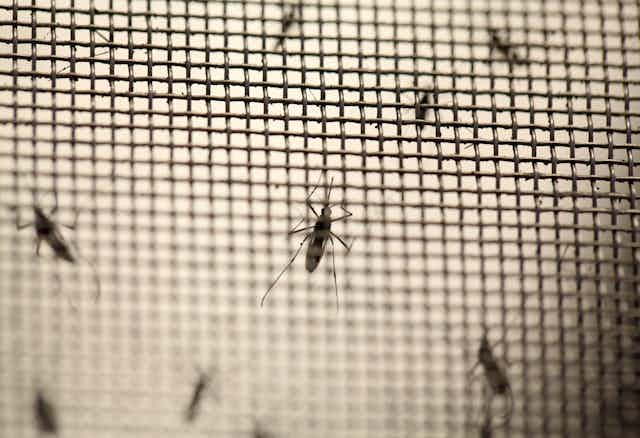
In the last 40 years of mosquito-borne viruses such as malaria, yellow fever and dengue, scientists have introduced myriad interventions to control the population of mosquitoes. This is because controlling mosquitoes has a large effect on controlling the diseases since the mosquito is the vector that carries them.
Novel mosquito-control approaches have included everything from deploying sterile male mosquitoes to soaps that could prevent people in high-risk malaria areas from contracting mosquito-borne diseases.
Zika, the latest mosquito-borne virus to be declared a global health emergency, has once again propelled innovations to tackle the control of mosquitoes.
There is talk of trying to stop Zika by giving mosquitoes a sexually transmitted disease and even injecting plants with a bacterium that would alter the mosquito’s genome and eliminate its thirst for blood.
Many of these innovations are good ideas but collectively they are only one of the tools in the armament of fighting mosquito-borne diseases. And they should not draw focus away from the tried and tested public health measures to control mosquito-borne diseases. These include environmental sanitation and access to clean water.
Different innovations
Making male mosquitoes sterile was one of the first innovations introduced in the 1970s when malaria was considered a problematic disease. This was becase the malaria parasite had become resistant to front line drugs.
Several other quick fixes have also been offered. These include fungi, worms and fish that parasitise and kill larval mosquitoes before they transform into adult mosquitoes. But these innovations were all found to be ineffective.
Changing the genetic makeup of the mosquito has also been explored. It results in mosquitoes that are not susceptible to the parasite. But this approach is still many years from application in field settings.
Having grown up on the banks of a heavily polluted canal in Nigeria and with limited access to potable water, the innovation that most fascinated me is a mosquito-repellent soap.
Two African scientists created the soap from natural oils and plants. The hope was that it could successfully prevent mosquito-borne diseases because it is cheap to produce and relies on existing habits such as bathing, cleaning and doing laundry.
But there is a catch. People need access to clean water to use the soap. Given that globally more than 700 million people still lack access to safe water, an innovation like a mosquito-repellent soap could become just another quick fix that only serves some but distracts from the complex task of providing more workable solutions.
The use of mosquito-repellent soaps is in fact not a new idea. Natural insect repellents have been in use for millennia and soaps containing such ingredients have been available for at least 30 years.
But natural mosquito-repellent soaps have been shown to have lower efficacy when compared to soaps containing the synthetic repellent DEET. More so, most of those natural ingredients could be harmful to health. Many of them cause cancer.
Some of these innovations have worked on a small scale but are not as effective on a larger scale. And although the innovations focus on mosquito control, this is only one of many factors that result in the spread of mosquito-borne diseases.
A complex set of diseases
The reality is that there are many factors responsible for the persistence and global spread of mosquito-borne diseases. These are complex.
They include:
insecticide and drug resistance;
changes in public health policies;
emphasis on emergency response;
demographic and societal changes; and
genetic changes in pathogens.
Climate change is also implicated. Since insects have no internal control over their body temperature, as ambient temperatures rise their distribution may expand through increased reproductive rate, biting behaviour, and survival.
Humidity and the availability of water for breeding in areas that are usually dry also promotes vector distribution and longevity. The incubation period of pathogens in vectors is temperature-dependent and becomes shorter in warmer conditions.
Unprecedented population growth, mostly in developing countries, has resulted in major movements of people, primarily to urban centres. This unplanned and uncontrolled urbanisation has led to inadequate housing and deteriorating water, sewage, and waste-management systems. These produce ideal conditions for mosquito-borne diseases to be transmitted.
My personal experiences and those of the hundreds of patients I treated for recurrent malaria in the slums of southern Nigeria are proof of this.
The best approach
So, what is the best way to prevent mosquito-borne diseases?
The variation in malaria’s epidemiology in and between countries shows that a multi-pronged approach is needed. This includes:
providing and improving public health infrastructure;
research to develop effective drugs and vaccines; and
improved vector control using proven techniques while taking up new innovations.
Research has shown that mosquito control measures built around environmental management are non- toxic, cost-effective, sustainable and highly effective in reducing morbidity and mortality. Those environmental measures including standing water, vegetation and drainage management all rely on access to clean water and sanitation.
The impact of adequate access to clean water, sanitation and hygiene go beyond mosquito control. They are essential for human survival. Access to these basic needs has a positive impact on the overall health, wealth and economic development of people and communities around the world.
Improving access to water also goes a long way in preventing – and even eliminating – other water and sanitation-related diseases such as cholera, trachoma, schistosomiasis, worm infestations and guinea worm disease.
UNICEF estimates that if countries in need were able to get basic, low-cost water and sanitation facilities, the world would save around US$263 billion a year. Those savings would come from obviated health and labour expenses.
The threats that mosquito-borne diseases pose to global health are as real as the are complex. The response must be broad and calculated. It must apply proven interventions while trying out new ideas.
Public health innovations should be considered as just one tool in our armament. They should not distract us, as they sometimes have, from the complex task of protecting and promoting global health through interventions like improving access to clean water, sanitation and hygiene.