The introduction into clinical practice of antibiotics is arguably the most significant medical advance of the 20th century. Together with immunisation and better public sanitation, they’ve had a significant impact on life expectancy. They’ve also allowed us to control infection, transplant organs, care for premature babies, treat cancer and have safe surgery and obstetric care.
In other words, they really are miracle drugs. Yet the use, overuse and abuse of antibiotics has led to drug resistance. And we’ve been failing to protect this precious resource.
A short history
Homo sapiens originated in Africa around 200,000 years ago. And we’ve had antibiotics for less than 70. In that time they’ve changed our relationship with bacteria, which have killed multitudes throughout recorded history.
The European population was halved by epidemics of smallpox, typhus and particularly plague – and the Black Death – between the 14th and 15th centuries; genital tract sepsis (due to streptococci) was the leading cause of maternal mortality in the UK in the 18th, 19th and early 20th centuries; and in 1812, Napoleon Bonaparte’s 665,000-strong army was reduced to 93,000 at the gates of Moscow by typhus (a louse-borne bacterial infection), before survivors struggled home with the bacterium to infect or kill another 2m.
A century ago, the three major causes of death in the US were tuberculosis, pneumonia and gastrointestinal infections.

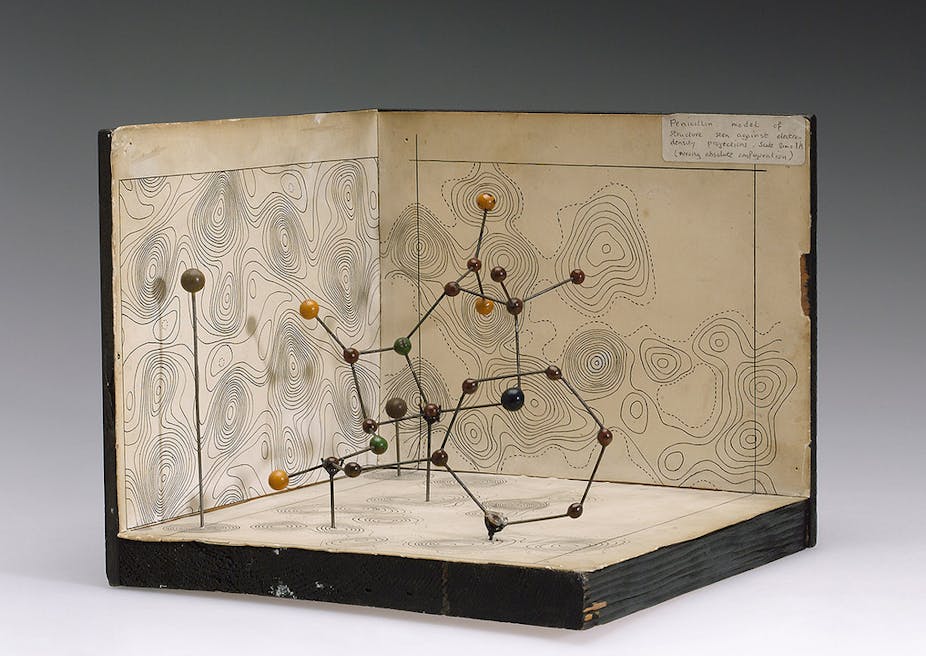
The discovery and commercial production of penicillin G in 1941 launched a golden age of antibiotic discovery and since then, potentially fatal bacterial infections have become easily treatable.
The fittest survive
Our thinking about most drugs stops at the clinical effects on our bodies and their toxicity. With antibiotics we have to consider a third party – microbes – which are able to adapt to what we throw at them. Bacteria, like other species, follow a selective process where the fittest survive and antibiotics make it more likely that those that do survive will be drug resistant.

This process is driven by the presence of antibiotics in patients and hospitals but also in the environment, for example when traces of antibiotics enter our food chain from the widespread use of antibiotics in farming. And it’s one of the few instances of human activity increasing, rather than decreasing, biological diversity.

We could well be on the losing side in our continual fight to outmanoeuvre resistant bacteria. Research and development of antibiotics is at the fringe of economic viability – considered uncompetitive compared with drugs for chronic conditions and “lifestyle products”.
Natural product research, which provided a starting point for the medicinal chemistry (as opposed to antibiotics that are derivatives of existing drugs), has also dwindled. A marine compound with antibacterial properties that was recently discovered was the first in decades.
What do we do now?
We can better control how we use antibiotics; not overusing them and using them properly when we do – not finishing a course of drugs can leave bacteria better equipped to fend of another dose in the future.
There are now alternatives to conventional antibiotic chemotherapy. Phage therapy, which uses bacteria-eating viruses to selectively attack microbes, is making a comeback. The technique was used before the advent of antibiotics and is now being reconsidered to fight antibiotic-resistant superbugs like MRSA (a meticillin-resistant strain of staphylococcus aureusis).
Rather than killing the invading bacterium, we could also disable it. The idea behind this is to modify the characteristic of the bacteria to make it “less fit” within the body in order that the immune system can eliminate the threat more readily.
MRSA: going into battle with green tea
Extracts of green tea contain a complex mixture of bioactive molecules that can improve blood flow and lower cholesterol. Its antioxidant effect can prevent cell damage and promote weight loss by increasing metabolic rate.

While its antibacterial properties are weak, epicatechin gallate (ECg) and epigallocatechin gallate (EGCg), complex chemical constituents of green tea, can alter the properties of MRSA by interacting with its membrane. The insertion of ECg in particular can cause a separation of two proteins that are essential for methicillin resistance, which makes it susceptible to drugs. This opens up the possibility of using ECg alongside methicillin or other penicillins that have lost effectiveness.
We could also help the immune system to remove dangerous invaders. We found an enzyme that strips away the capsule from Escherichia coli K1, one of the major causes of bacterial neonatal meningitis. Administration of very small amounts of the enzyme led to prevention and cure of the infection, provided it was given early enough.
Many different bacteria can cause septicaemia (infection of the blood) or sepsis (inflammation of the blood circulation) – a major infectious killer of newborn babies – when normally harmless bacteria gain entry to the blood through sites of colonisation on the skin or mucous surfaces during or shortly after birth. Those that get into the central nervous system to cause meningitis have a protective external capsule. Removing the protective capsule could, therefore, prevent these dangerous pathogens from causing infection.
But E. coli is only one of a number of bacteria that cause meningitis in newborns so the enzyme isn’t likely to be developed further. However, an ideal infection for this “capsule-stripping” approach is anthrax because a sole pathogen (Bacillus anthracis) producing an invariant, unique and essential capsule is responsible for the disease.
Waking up
We are at last waking up to the threat of resistance. There is now a high level of concern about the issue and a greater willingness to develop new ways to treat infections. In UK, the implementation of basic infection control measures has contributed to a reduction in incidence of MRSA and C. difficile. There is also, finally, a renewed interest in antibacterial drug discovery (driven by a commitment to more funding).
Antibiotics are the greatest drugs ever developed but we can’t continue to use them as we have without better management. And we now need to look at fundamentally new ways to counter the present threat of bacterial infections in our hospitals and, increasingly, in our communities.