Hollywood actress Angelina Jolie Pitt has revealed in the New York Times that she had her ovaries and fallopian tubes removed to prevent ovarian cancer. Two years ago she underwent a double mastectomy and breast reconstruction after she was found to carry a mutation, or alteration, on the BRCA1 gene. This was inherited from her mother, who developed ovarian cancer aged 49.
The BRCA1 and BRCA2 genes were first identified more than 20 years ago. They can increase the risk of breast and ovarian cancer, if a person carries an alteration in one of these genes. The risk of breast cancer with BRCA1 and BRCA2 is around 50-80% over a lifetime and around 10-50% for ovarian cancer.
In addition to knowing she had alteration on her BRCA1 gene, Jolie Pitt also had other tests to monitor for signs of early cancer. These included an annual check for elevated levels of the protein CA-125 in her blood. She said she had been planning on removing her ovaries for some time but opted to have the operation sooner after other tests revealed an elevated “number of inflammatory markers” that could be together a sign of early cancer.
The salpingo-oophorectomy
Jolie Pitt’s decision to undergo a laparoscopic bilateral salpingo-oophorectomy – when both ovaries and fallopian tubes are removed using a fibre-optic camera and surgical tools inserted through several small incisions in the abdomen – was linked to her family history. Her mother, grandmother and aunt all died of the disease. As she put it: “I know my children will never have to say, ‘Mom died of ovarian cancer.’”
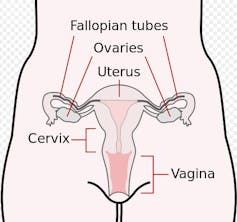
Up to 70% of female BRCA carriers, like Angelina, opt for this kind of surgery, which reduces the risk of developing ovarian cancer by around 95%. It is usually offered to women who are at high risk of developing ovarian cancer but have completed their family – and not usually before the age of 35-40. If this type of surgery is carried out before a woman is 45 it can also reduce her risk of getting breast cancer. There is a small risk of complications including bleeding and infection, but women can return to full activity after two to six weeks. However they will enter the menopause early afterwards and will be offered hormone replacement therapy.
However, as Jolie Pitt acknowledged, there are different options out there for women who are at risk of cancer through a mutation in one or both genes. Options include monitoring signs of early cancer, or removing fallopian tubes but keeping ovaries, which would leave the option for having more children or avoiding early menopause.
Tests, drugs and screening
Breast MRI scans are carried out annually in the UK for women between the ages of 30 and 50 (and mammograms from 40). But extra breast screening is offered to women in the who carry a BRCA gene alteration.
We still don’t know how far drugs can prevent cancer developing in BRCA gene carriers. Tamoxifen, for example, can help protect against breast cancers that respond to the female hormone oestrogen, but data on its use in BRCA carriers is limited.
Ovarian screening is unproven. Research studies such as UKFOCSS (the UK ovarian cancer screening study), which recruited 5,000 high-risk women to an ovarian screening programme where they were offered annual ultrasound and CA-125 blood tests, has not yet shown any definite benefit in detecting the cancer early. Symptoms of ovarian cancer are non-specific, and often diagnosis is delayed.
A number of research groups are looking for new markers for ovarian cancer to improve detection, such as the PROMISE 2016 project at UCL’s Institute for Women’s Health. These tests are not yet ready for clinical use.
The contraceptive pill and tubal ligation (where the fallopian tubes are cut or tied in a woman who has completed her family) may reduce ovarian cancer risk, but for BRCA carriers this risk remains significantly increased.
Testing for BRCA1 and BRCA2 is becoming more widely available, and women who have breast or ovarian cancer may not need a family history to be offered genetic testing. This group includes women under 50 who have a type of breast cancer called triple negative, and women with high-grade serous ovarian cancer. The outlook for women with BRCA gene alterations will improve, with greater access to genetic testing and screening and risk reducing surgery for women who have not yet developed cancer.
As Jolie Pitt said, there are options but not easy decisions, and “you can seek advice, learn about the options and make choices that are right for you.”

