People constantly encounter viruses, bacteria or parasites. Fortunately, our skin, the specialized lining of our guts and other parts of our body that are exposed to the outside world prevent them from entering. When a pathogen breaches this barrier, our body’s defences come into play.
Those defences, which we also call the human immune system, have two branches — innate and adaptive. Our innate immune system is our first line of defence. It has special molecules that recognize “fingerprints” or patterns in proteins or genetic material that are only present in pathogens. These molecules signal the presence of a pathogen to the cellular genetic machinery, which then produces effector molecules called cytokines.
The effector molecules initiate a process to eliminate the pathogen. The adaptive immune response kicks in at a later stage. Its job is to mount a much more robust defence by destroying cells infected with a virus or by neutralizing the virus or toxins produced by bacterial pathogens.
The adaptive system also has a memory and activates very rapidly if it encounters the same pathogen again. The innate and adaptive immune systems are linked and the innate system primes the adaptive branch of immunity for a more robust immune response.
Response against invaders
The innate immune system is primitive and probably evolved earlier in invertebrates and lower vertebrates. Although innate immune response has systemic effects on the entire human body, every cell can be considered a factory housing some components of the innate immune response.
Innate immunity starts at the cellular level through conserved pathogen sensing proteins in the cell that sense a pathogen, such as a virus. During virus infection, sensors in human cells recognize viral proteins and nucleic acids to activate genes, such as interferons that inhibit viral replication.
Once infected cells have sensed an invading pathogen, they secrete molecules called cytokines and chemokines. Cytokines such as interferons are molecules that signal neighbouring cells and induce an antiviral state in them. These cells are then primed to resist an infection with the invading virus. Cytokines such as interferons activate anti-viral genes in the infected and neighbouring cells. These genes are called interferon stimulated genes (ISGs) since they are only made in the presence of interferons. ISGs impede virus replication in the cells.

At the tissue level, an infection usually manifests itself in the form of an inflammation. Typical signs of inflammation include redness, swelling, pain, heat and loss of function. This is an area of intense battle between the invading microbe and the body’s immune system. Each cell within this area is like a soldier and several cell types together form an army against the microbes.
Chemokines are molecules that attract specialized immune cells to this site of infection. These include cells that “eat” pathogens and dead cells such as macrophages. In the battlefield, chemokines are like “radio calls.”
Macrophages respond to these calls and invade the site of infection, consuming any cell-free or cell-associated pathogen. These pathogens are then destroyed by internal mechanisms in the macrophages. Macrophages are also like the medics in a battle zone. They help remove damaged cells (“wounded soldiers”) and clear the area.
White blood cells such as neutrophils respond to chemokines by migrating to the site of infection. These cells secrete powerful inflammatory molecules and reactive oxygen species that aid in getting rid of the pathogen.
Neutrophils, just like macrophages, can also ingest microorganisms or particles. Neutrophils are cells that have internal granules that house powerful chemicals. When neutrophils accumulate at the site of infection, they release these chemicals that have bactericidal properties.
An evolutionary battle
Pathogens continue to evolve new mechanisms to evade the body’s immune response. Charles Darwin’s theory of evolution and survival of the fittest are relevant for microbes as well. Just like bacteria evolve to become resistant to antibiotics, viruses evolve ways to evade the immune responses.
Coronaviruses have evolved mechanisms to shut down cytokine production. In the absence of cytokines, the cell has no way to communicate with other cells about the viral infection. The virus can then multiply to higher levels, causing significant infection and even death in humans. This has been observed both in severe acute respiratory syndrome (SARS) and Middle-East respiratory syndrome (MERS).
It’s therefore very important to identify the mechanisms employed by these viruses to shut down host defences. Drugs can then be designed to inhibit these viral mechanisms and boost human innate immune responses.
The innate immune system has control mechanisms to inhibit damage to the human body by excessive secretion of cytokines. Cytokines are deemed necessary for controlling virus replication, but excessive production of cytokines leads to tissue damage. Excessive cytokine production, a phenomenon called “cytokine storm” in SARS patients has been associated with lung damage. So a timely balance between inflammatory and anti-inflammatory processes is ideal to tackle infections.
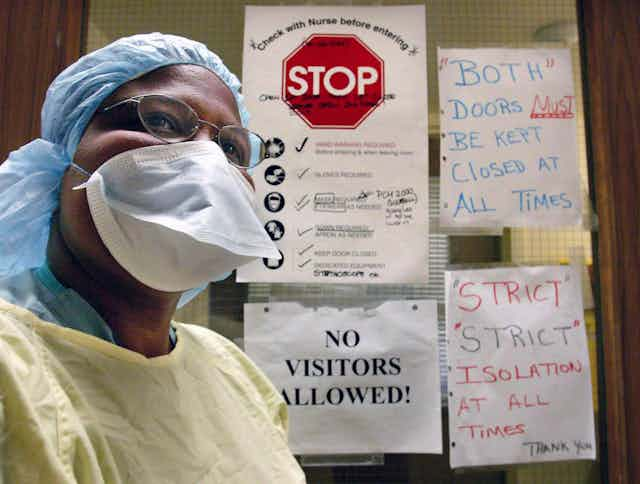
The innate immune response is really the sentinel of the human body; standing at the doors to detect invading pathogens. These sentinels fight off an invading organism while alerting the adaptive immune response (“the cannons”) about the threat.