Freezing eggs is extremely unsuccessful. Although it’s never admitted, it is true from the national statistics, how poor the chances of pregnancy are afterwards.
Lord Robert Winston, speaking on BBC Radio 4’s Today programme on November 1.
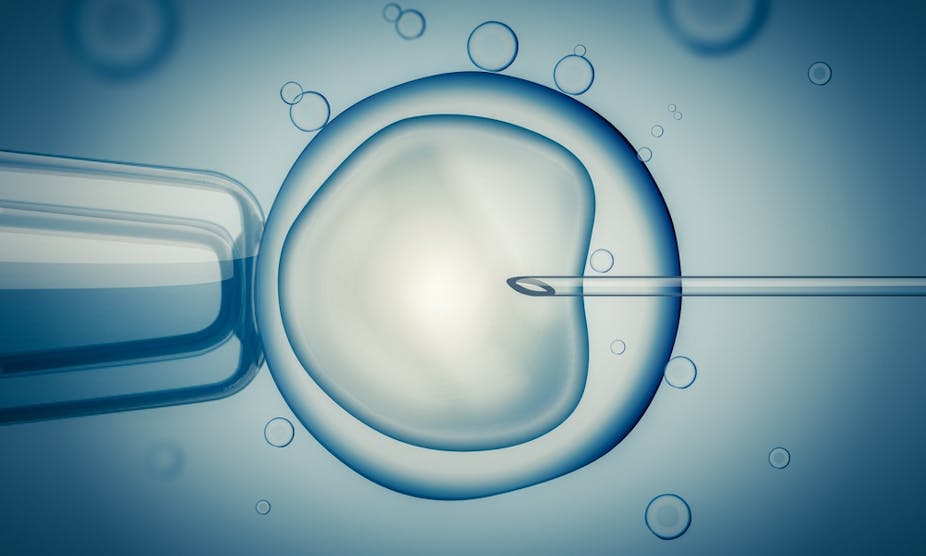
In the UK, if a woman wants her eggs frozen, she is given a course of drugs to help increase the production and maturity of her eggs. About 15 eggs are collected for freezing, preferably using a fast-freezing process called vitrification, which is thought to be more effective than slow freezing.
Freezing can preserve eggs for up to ten years – this is the time-limit placed on storage by the Human Fertilisation and Embryology Authority (HFEA), the agency that regulates fertility treatments in the UK.
The cost of freezing eggs in the UK ranges from £2,500 to £5,000 (plus storage fees).
Despite the fact that the process of freezing eggs seems to be increasingly effective, it nevertheless appears that fertility expert, Lord Winston, is correct when he says that freezing eggs is extremely unsuccessful, given that the birth rate using these eggs is about 14%. But there’s more to the story.
The low success rate Lord Winston appears to be referring to is the number of live births that result from thawing frozen eggs. His office pointed The Conversation to a written question he recently submitted in the House of Lords on the issue.
The truth is that fertility experts are actually quite good at freezing eggs. It is the combined processes of thawing them – at which point some don’t survive – and then using in vitro fertilisation (IVF), that makes the success rate so low. But IVF isn’t that successful even when fresh eggs are used (about a 27% success rate).
And there’s more to the story. While the HFEA reports that the number of women freezing their eggs has risen year on year, the number of frozen eggs that are thawed and used in IVF, in the UK, remains very low. This means that not only is the 14% success rate based on a small sample, it may also reflect the fact that doctors in the UK don’t get much practice at conducting this procedure.
So, although the current success rate is low, it is likely to improve with time. Women who freeze their eggs now may see success rates increase by the time they want to use their eggs. And for many women – including those undergoing chemotherapy – freezing their eggs offers a glimmer of hope that wouldn’t have been possible a little over three decades ago.
Verdict
So Robert Winston is right, in a sense, but, as always, there is more to the story.
Review
Sarah Martins da Silva, consultant gynaecologist and senior lecturer in reproductive medicine, University of Dundee.
It’s not difficult to agree with this verdict. And John Appleby is right to point out several fundamental issues with Lord Winston’s opinion that freezing eggs is extremely unsuccessful.
Egg freezing has been used since the late 1990s for women of a childbearing age about to undergo chemotherapy or radiotherapy. But eggs are notoriously difficult cells to preserve using traditional freezing techniques due to their low surface-area-to-volume ratio, and high risk of ice-crystal damage. And poor egg survival resulted in low pregnancy and live birth rates using these slow-frozen eggs in fertility treatment ten to 15 years ago.
However, assisted reproduction is a fast-moving speciality, and the introduction of vitrification (the fertility laboratory equivalent to freeze-drying) was a game changer. By late 2012, the American Society for Reproductive Medicine and Society for Assisted Reproductive Technology announced that egg freezing was no longer considered an experimental technique. This followed results from four randomised controlled trials that demonstrated that IVF using vitrified/warmed eggs produced similar fertilisation and pregnancy rates to IVF using fresh eggs.
While egg vitrification was initially reserved for fertility preservation for women with serious medical problems, it has evolved to play an important role in fertility preservation for transgender people, egg preservation for egg donor programmes, and – perhaps more controversially – “social egg freezing”, whereby a woman chooses to freeze her eggs with a view to deferring having a family rather than a medical need to do so.
It’s also worth noting that serious female illness is associated with poorer egg quality, which reduces success of fertility preservation treatment. This is independent from the technology applied to freeze eggs, but one which continues to significantly influence data on outcomes from egg freezing in this group of women. Conversely, the largest series to date of over 3,500 egg-recipient treatment cycles using vitrified donated eggs from healthy women, shows a thaw survival of over 90% and a clinical pregnancy rate of 48%.
The author is correct: the UK has relatively limited experience of fertility treatment using vitrified eggs. But the global viewpoint is that this is a robust technique and a valid option, although certainly not perfect. Numbers are just too small to judge egg freezing as “extremely unsuccessful”.